
Next you will find out:
- What symptoms are usually accompanied by rejection of the implant and when it can start the problem;
- How long implants take root and why are they sometimes rejected;
- What sensations should be considered the norm after the operation just performed, and which - signs of dangerous inflammation in the area of the implant;
- What to do if inflammation has begun and whether reimplantation is possible after rejection of the implanted structure.
... And also some other interesting and important from a practical point of view nuances concerning the problem of implant rejection.
It should be understood that the implantation of teeth is a rather complicated and to some extent traumatic procedure, the healing process of tissues after which does not always proceed smoothly: swelling, bleeding, pain due to gum and jawbone are possible.However, all of this is the normal consequences of a surgical intervention, which disappear on their own in a few days.
But there are also complications that require a doctor’s surgery. And, perhaps the most unpleasant of them is the rejection of a tooth implant. The first symptoms of this problem are, as a rule, acute pain, the mobility of the structure, the appearance of an unpleasant odor, as well as redness and swelling of the mucous near the outer part of the implant (abutment, cap).

Generally speaking, the rejection of implants today is quite rare, and patients do not need to pre-tune in to the adverse outcome of the operation. However, it is necessary to know the characteristic signs of incipient rejection, to understand what inflammation can undergo under the implant - it is always useful to be prepared for possible complications in theory in order to prevent their occurrence in practice.
We will discuss this further in more detail.
How long do implants usually take root and when can they be rejected?
The average period of implant engraftment is about 2-4 months at the lower jaw and about six months at the top.This difference is due to the fact that the bones of the mandible are better supplied with blood, they are generally larger and stronger, they have a higher chewing load. In addition, above the bone tissue of the upper jaw is the nasal sinus, the proximity of which often introduces additional difficulties when installing implants.
Osseointegration (this is a medical term for the process of accretion of metal roots with the jaw bone) begins immediately after the installation of structures. The time of engraftment largely depends on the initial state of the jaw bone, as well as on the quality of workmanship and the model of the implant itself.
At the same time, the method by which implants were installed in the jaw does not play a special role. Regardless of whether the implants are loaded immediately (for example, during a basal implantation), or only after full adhesion with the bone - in both cases, the time of engraftment does not differ much.
According to statistics, if the rejection of implants occurs, in most cases this is observed in the first days after their installation. In other words, if something went wrong, the first symptoms of a complication, as a rule, do not take long to wait.
However, the patient should not lose vigilance and after the successful engraftment of the structure - inflammation after dental implantation with subsequent implant rejection may overtake even after several years of active use.
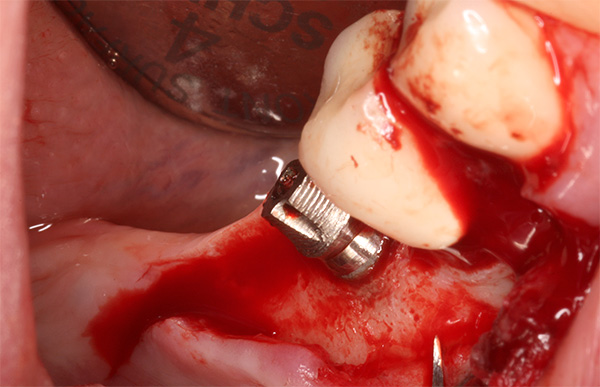
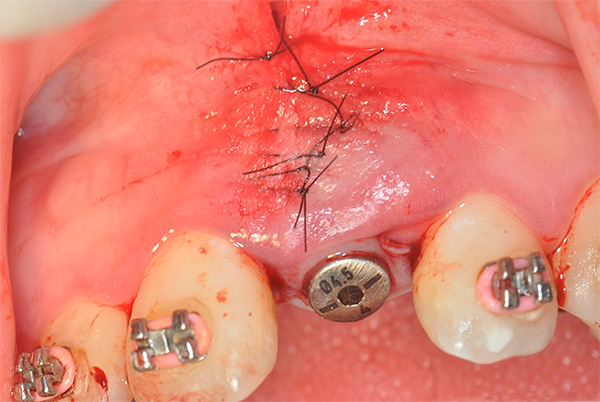
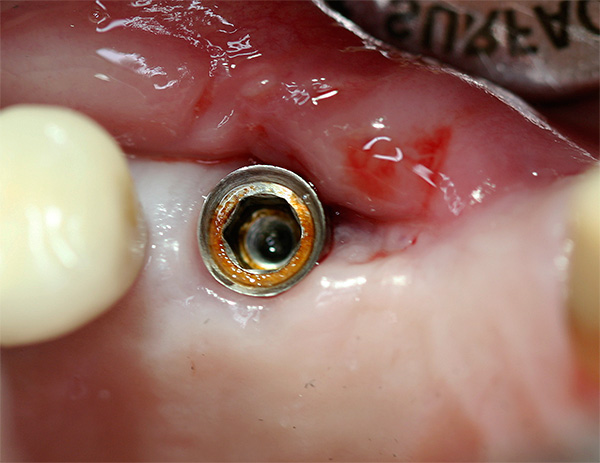
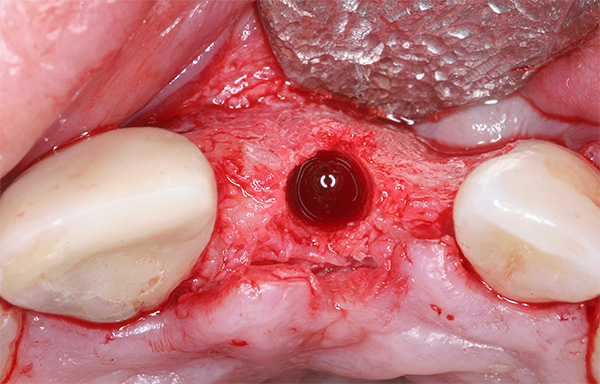
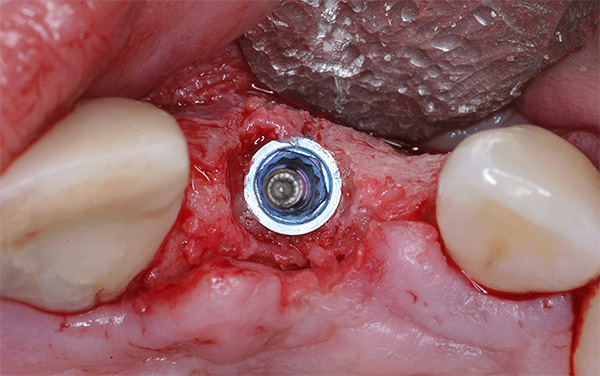
The photo below shows a relevant example (inflammation began 10 years after the implant was installed):

Below we will see what can be done to avoid this adverse outcome. However, before this, let's talk about what sensations to consider as the norm after dental implantation, and what should be perceived as periimplantitis symptoms that threaten to escalate into implant rejection.
On a note
Periimplantitis is called inflammation of the tissues adjacent to the implant - these can be either soft tissue or bone tissue. If the inflammatory process is not prevented in time, these tissues will gradually begin to collapse and the implant will become mobile - in fact, it will be rejected.
Signs of dental implant rejection
After the implantation procedure, you will often have to visit your doctor in charge: the first appointment will take place already on 2-3 days after the implants are implanted.Such examinations are very important for the timely detection of possible problems (it was already mentioned above that in the case of rejection of the implanted structure this process often takes place in the first days after the operation, so at this stage the monitoring should be especially careful).
The dentist will evaluate the stability of the implant and the condition of the tissue around it. On examination, it will become clear how well the structure fuses with the bone, whether there are signs of dangerous inflammation and whether additional intervention is required to prevent unwanted complications.
Let's first see what unpleasant symptoms are considered normal after implantation. Since the implantation of implants is associated with tissue injury (even in the case of basal implantation using the puncture method), after the operation, there are always more or less marked discomfort and corresponding external signs:
- swelling of the gums (sometimes the entire cheek swells);
- redness of the gums;
- jaw soreness in the area of the installed implant.
On a note
These effects of surgery normally pass fairly quickly, after 3-4 days (maximum - in a week).If you feel severe pain all week, but it does not go away or even increases - this is a sure sign that healing is not fast enough. By the way, whether it comes to the rejection of the implant, or it will be all right - it often depends not only on the doctor, but also on the actions of the patient himself (more on that below).
However, in some cases, for example, with simultaneous bone grafting, as well as in the presence of acute inflammatory processes in the hole, the rehabilitation process can take up to a couple of weeks.

Now consider what symptoms indicate a deviation from the course of normal rehabilitation after the installation of implants.
Generally speaking, some of the symptoms of rejection of a dental implant (or periimplantitis - inflammation of the tissues around the structure) are in many ways similar to the usual postoperative effects. However, they are usually more pronounced and persist for a long time:
- acute pain that does not go away within 1-2 weeks after implantation;
- swelling and redness of the gums that lasts more than 4 days after surgery. Even in the most difficult cases, the swelling subsides within 3-4 days,so if it lasts longer - this is an alarming sign;
- prolonged bleeding from a wound, as well as prolonged discharge of the so-called exudate (ichor). If such discharge lasts more than 7 days, it is not very good;
- the mobility of dental implants - here in many cases it is possible to immediately predict that the structure is unlikely to take root in the future;
- if there is an unpleasant smell under the plugs installed on the implants;
- pus from the gums - an abscess can be located next to the implant and communicate with the inflammation through the formation of a fistula, or pus can go directly from under the implant (sometimes there is an unpleasant smell from the mouth);
- soreness when pressing on the implant is a very characteristic sign that there are serious problems with the integration of the structure. In such cases, it is better not to expect that everything will pass by itself and “resolve”;
- fever.
All the listed symptoms may indicate a possible rejection of the implant, their appearance at any stage of treatment requires immediate consultation with a specialist.

"Inflammation of the implant" of the tooth (or more precisely, the surrounding tissues) can proceed without symptoms, especially several years after the implantation of the structure in the bone. The patient may not pay attention to a slight pain and redness of the gums - a pronounced reaction to implant rejection may be absent, and inflammation in the meantime will lead to the destruction of bone tissue and, consequently, an increase in the mobility of the implant.
This situation is further complicated by the fact that later an additional operation will be required to restore the jawbone before re-implantation.

It is interesting:
On average, implants are rejected in no more than 3-5% of all cases, and the rates vary greatly depending on the brand of structures. For example, German or Swiss-made implants successfully take root in 97-98% of cases, and more affordable Israeli or Russian-made products - about 95%.
The photo below shows an example of tissue inflammation in the area of an installed implant:

Why are dental implants sometimes rejected?
The reasons for the rejection of dental implants in general are not so much.In most cases, the problem occurs by mistake of the doctor during the procedure. Much less often - when choosing a poor quality or even a fake implant (again, this can also be considered a medical mistake).
But the patient shouldn’t relax either - due to the peculiarities of the state of health or non-observance of certain rules of behavior in the rehabilitation period, dental implants can also be rejected. Symptoms of the onset of rejection in almost all cases will be the same, regardless of the reasons for them.

Consider the possible causes of problems in more detail.
The first reason: lack of professionalism or a doctor’s mistake
A characteristic feature in this case is that the implants begin to reject immediately, that is, during the engraftment period.
Unfortunately, dental implants are rejected most often because of medical errors - this may be a lack of experience, especially when dealing with complex clinical cases, lack of professionalism, or just plain inattention.

Here, for example, what mistakes an implantologist can make while working:
- incorrectly chosen implant design - for this reason, the implant may not be able to properly fix in the bone(for example, it may be noticeably longer or thicker than bone tissue);
- lack of sterility of the working tool or working area in the oral cavity (the centers of acute inflammation were not eliminated) - as a result, an infection is initially present in the wound;
- overheating of the tissue when drilling the hole for the implant;
- incorrect positioning of the implant in the jaw;
- the lack of sufficient information about the patient's state of health — possible contraindications are not excluded.
A particular difficulty for the doctor is the lack of sufficient bone tissue to secure the implant (for example, due to its atrophy) and acute inflammatory processes.
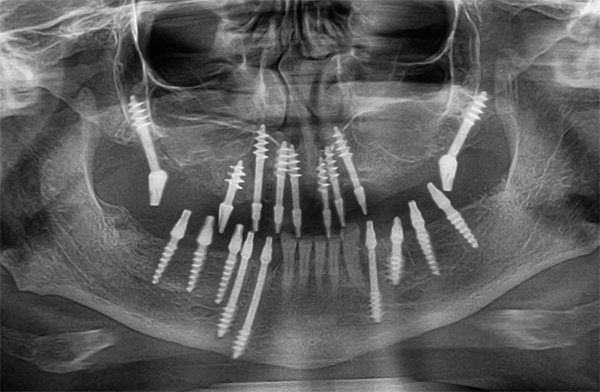
The problem of bone atrophy can be solved by its replanting or the choice of the method of basal implantation, in which special design implants are used, which are fixed in the deepest basal parts of the bone tissue. However, rejection of basal implants can also occur at any stage of engraftment. According to statistics, they have to be removed no less than classical implants.
On a note:
Implantation for periodontitis and periodontal disease, that is, against the background of acute inflammation of the gums, associated with the destruction of bone tissue, is quite possible today.But to install implants in the presence of such inflammatory processes, not all implantologists will decide. Basically, a similar procedure is carried out simultaneously with the removal of the patient's tooth, and after implantation of the implants, drug therapy is prescribed with simultaneous enhancement of oral hygiene.
When implants are rejected due to acute inflammation of the jaw tissues, repeated implantation is not always possible due to severe destruction of the bone.
The second reason for possible rejection: poor-quality implant
Large dentists work with dealer networks that supply implants directly from the manufacturer, which eliminates the possibility of obtaining fakes. In small clinics, the situation is more complicated.
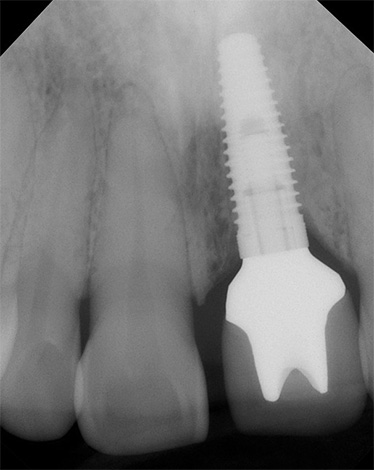
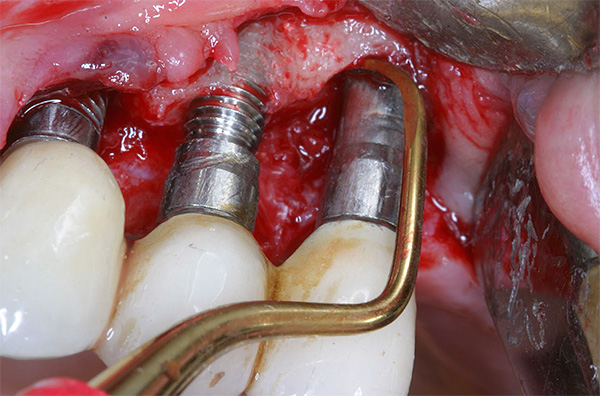
The photo below shows an example of corrosion of a poor-quality implant:
The quality of the implant itself also plays a big role: the more expensive the system is, the more advanced materials and technologies, as a rule, are applied in the manufacture of the structure. For large implant companies, large budgets are spent precisely on improving products and developing innovative technologies.
It is interesting:
The quality of engraftment, and hence the risk of possible rejection, largely depends on the material from which the implant is made (it should be biocompatible with our body titanium), as well as on the characteristics of its surface. Today, many manufacturers prefer the porous coating - growing cells of the jaw bone penetrate into it, which ensures a strong adhesion of the bone and implant.
The third reason: violations by the patient
In this case, the symptoms of implant rejection may appear both during the engraftment period and after a few years of using new teeth.
It should be borne in mind that even if the doctor performs all his work on installing the implant perfectly, the wrong follow-up actions of the patient can negate even the best result of the treatment. What you need to pay attention first of all:
- implant should not be loaded during the engraftment period;
- overheating and overcooling of the body in the first days after the operation is prohibited (that is, one cannot go to the bathhouse or dive into ice water - all of this can weaken the immune system to some extent);

- you do not need to hide the existing health problems from the doctor - it can be life threatening, although you yourself may feel that these problems do not have a relation to the implantation of teeth and you can keep silent about them;
- if the doctor prescribes, then it is necessary to take disciplined preparations against the rejection of implants - the means prescribed by the doctor can speed up the healing process and minimize the risk of periimplantitis;
- it is necessary to take care of new teeth - to brush in the morning, in the evening, to remove food debris after eating (some people think that since these are artificial teeth, they “do not rot” and do not need care - and this is a big mistake);
- highly desirable to give up bad habits - in particular, not to smoke.
On a note:
Practice shows that smokers have dental implants rejected more often than non-smokers. According to statistics, approximately 30% of patients who smoke have symptoms of rejection already observed during the first five years after surgery. As a result, implants have to be replaced with new ones.
Toxic tar and nicotine lead to malnutrition of mucosal cells, which has a very negative effect on the state of the tissues around the implant.Ultimately, the design loses its stability, becomes mobile, rejecting the body.
The question is: what do smokers do? The choice is not very large - either to refuse implantation, or to reconsider your lifestyle - stop smoking (or at least smoke less often).
The fourth reason leading to the rejection of dental implants: poor health
This reason leads to the rejection of implants mainly a few years after their installation.

If the implants are not rejected in the first two years, then we can safely talk about the success of the treatment. But the problem may arise many years after the installation of structures. This is extremely rare and is mainly due to either mechanical injury, or aggravation or the development of certain diseases: cardiovascular, diabetes, immune (AIDS), tuberculosis, or cancer.
What to do if inflammation starts under the implant?
When anxious symptoms of inflammation begin to appear in the area of the installed implant (there is a smell from under the implant, pain, redness of the gums, swelling, etc.) appear, the only right decision would be to go to a doctor immediately.The implantologist will conduct a visual inspection of the condition of the installed implant, make an X-ray examination, and, if necessary, open the gum and help clean the wound from pus.
If problems began even during the period of engraftment of the structure, sometimes the cause of discomfort (for example, the putrid smell from the implant) is easily solved by temporarily unscrewing the implant plug and cleaning its outer surfaces.
But in the presence of clear signs of periimplantitis, in most cases, removal of the installed implant is shown, and this should be done as soon as possible. Indeed, otherwise, the started inflammation can lead to the spread of infection throughout the body, which is fraught with very serious consequences, even to the threat of the patient's life.
In addition, the longer the inflammation in the area of the implant is observed, the more the bone tissue around it is destroyed, and the more there may be problems in the case of re-implantation.
Is re-implantation possible after implant rejection?
Repeated implantation is possible in most cases. This should take into accountthat after removal of the rejected implant, no more than 1-2 months should pass - otherwise the bone tissue, without receiving the proper load, will gradually atrophy.
If necessary, bone grafting can be carried out and drug therapy can be prescribed to suppress the infection at the site of inflammation. After the restoration of damaged tissue is re-implantation.

On a note
According to the law, there is no guarantee for surgical work, so the patient will have to rely on the consciousness of the administration of the clinic or the doctor, who will fulfill their own independent warranty obligations. The long-term or unlimited warranty on implants, which is set by the manufacturers of the structures, is just the lifetime of artificial teeth. But whether they will serve the declared years - it depends on the patient and the doctor.
How can you protect yourself in advance from possible problems associated with implant rejection
In conclusion, it is worthwhile to cite a few useful tips that will minimize the possible problems associated with rejection of installed implants.

So, here are these tips:
- you should realize in advance that the responsibility for the result of treatment lies not only on the shoulders of the doctor, but also on you (the undisciplined patient, who does not follow the instructions of the doctor, can spoil the results of even the most jeweler's work);
- choose a clinic with a “name” - as a rule, large centers invest in modern equipment and staff training;
- choose a professional doctor who has experience and positive recommendations and feedback (the choice of a doctor is more important than the choice of a clinic);
- give preference to high-quality implants - not lower than the average price segment (you should choose well-known brands that exist on the market for at least 5-7 years);
- comply with all the requirements of the doctor after the operation and monitor oral hygiene;
- and, of course, do not forget to regularly undergo preventive examinations of the oral cavity, timely treat diseases of the teeth and gums and take care of them daily.
In general, the risk of falling into the number of patients whose implants are rejected is minimal. It is much more likely that they will serve you faithfully for many decades, or even a lifetime.
An interesting video about the complications that may arise during the implantation of teeth.
What to choose: implantation or crowns?




Not 2 years have passed. A mini maxillary implant causes pain and swelling in the wing of the nose and cheekbones in the maxillary sinuses. Prosthesis removed. What to do?
Hello! You need to contact an experienced implantologist as a matter of urgency. To do computed tomography. Judging by the description, the mini implant became mobile and could damage the bottom of the maxillary sinus, this is indicated by pain in the wing of the nose. If my suspicions are confirmed, then the implant will need to be removed and the inflammation removed. And after removing the threat of the spread of infection to see how to further restore teeth. Personally, I do not recommend the installation of needle mini-implants, since they do not have good primary stabilization in the bone, it is simply not possible to achieve because of the structural features of the product itself. As a rule, the prosthesis incorrectly distributes the load, which leads to the mobility of the implants and serious damage to the bone tissue around them. Often such implants are rejected and “fall out”.
After implantation in the upper jaw of 3.4 teeth, expectora appears from expectoration from the nasopharynx. The time after implantation is three days. At the doctor's appointment to remove the stitches in four days. What to do, go to the doctor before?
Good afternoon, I don’t know if you had a sinus lift operation or if the implants were installed immediately (in the latter case, the bottom of the maxillary sinus could really be damaged). See your doctor right now and do a CT scan to see what is going on. Spotting from the nasopharynx is a sign of complication. I hope you strictly adhere to the instructions of the doctor after sinus lifting, if there was one. The patient should not rinse his mouth in the nasopharynx within 3 days after the procedure, do not hark, not blow your nose, try not to sneeze, drink through a straw.
Hello, Doctor. I had an implantation 11 days ago with a simultaneous increase in bone tissue. The stitches have already been removed.
1. Edema was and stayed for a week. Now in the gum, where there are implants, barely noticeable swelling, to the touch clearly noticeable.
2. At first, it was bleeding for several days, then it was replaced by some discharge, with a yellowish-white color. At the moment they are still there, little by little they come out. My implantologist says that this is bone tissue, i.e. formation of bone tissue.
3. Along the edges of the gum is slightly raised, and the next tooth aches when tapping it.
Questions:
1. Are the periods of edema normal under this condition and how long can they hold? 2. The discharges described above are a normal process and how long will they last? 3. Is the gum and tooth all right?
Implantologist-author says that these are all normal processes, I want to believe, but, as they say, trust but verify.
Thanks in advance for the answer.
Hello!
1. Edema and pain are normal after a sinus-lift operation, as a reaction to a tissue injury. Up to 10 days can be maintained if the injury area is large.
2. Discharges cannot be called the norm, but here it is necessary to know more clearly the clinical picture of the TO in order to assert precisely. Without a survey it is difficult to say when it will stop.
3. What hurts a nearby tooth is normal and will pass with time. Some time passed and not all tissues were rehabilitated.
If you want to check exactly whether everything is in order, contact another doctor - today many clinics provide free advice. When choosing a doctor, try to find a person with experience, preferably a periodontal implantologist, or an FLA.
Hello, I have an Israeli implant, installed 5 months ago. Around the implant are formed, as the doctor called them, - bedsores, he says that such a process is possible if many years have passed, but not 5 months. When he puts the shaper gums, then pressure on him is sick. For some reason, the former had been twisted for the last couple of days, and I had a feeling that it was being squeezed out. I push him there, and after a while he climbs out. How is implant rejection?
Good day. If there is pain in the area of the implant when biting and pressing, then it is highly likely that you have already started the process of periimplantitis. But without a snapshot here you can’t say 100%, this is a tentative answer. Regarding the shaper gum - also need inspection. It is possible that the shaper is not correctly selected, or it is not sufficiently twisted. Definitely it can be said that the behavior of the former is atypical.
I recommend that you urgently consult a doctor and do a CT scan to examine the condition of the bone tissue in the area of implantation and, if necessary, take timely measures to curb the inflammatory processes.
A week after the basal setting, a painful bump appeared under the chin. What is it?
Hello, Nilea. After implantation with immediate loading, phenomena such as swelling or bumps in the chin area are possible, but very rarely. However, do not be afraid that the implant can be torn away. Since the basal implant is polished and installed in deeper sections of bone tissue, the probability of problems with it is very low. Perhaps this is a reaction of the body (more precisely, the surrounding tissue around the implant), manifested by compaction of the periosteum.
I recommend to go for a checkup to the doctor who installed the implants for you. I would also advise you to do computed tomography of the chin department and make sure that there are no serious changes in the form of bone loss around the implant.
A week ago there was an implantation, tonight the temperature suddenly rose 37.3. Five implants were placed, around the two gums are still swollen and blood is seeping from under the formers. The surgeon is on vacation and will be only in a week.What to do is not clear, there is no second implantologist at the clinic.
Hello Tatiana! The recovery period after surgery may take up to 3-4 weeks and includes a little discomfort. In some patients during this time, some pain and swelling of the postoperative area remains.
Now in your situation it is necessary to turn to any dentist (it is advisable not to wait for one), regardless of his specialty. That is, in fact, you can contact any dental clinic for an examination in the oral cavity and, possibly, a computed tomography (CT), the results of which will allow you to understand the true cause of your symptoms.
I would also recommend focusing on improving oral hygiene, since against the background of a decrease in local immunity after surgery, one of the causes of complications is often unsatisfactory cleaning of the oral cavity. If the temperature does not decrease, and the blood continues to flow, then, most likely, the installed implants were infected. Since your doctor will surely be back from vacation by then, you will need to contact him immediately.
Hello. Installed implants, 5 and 6 below.It hurt for 7 days, then calmed down. After 10 days, the stitches were removed, the surgeon said that everything was fine. 3 days after the stitches were removed, the pain started, severe. The whole jaw ached, it seemed that all her teeth were inflamed: above and below. They took a picture, opened the 4-ku next to the implant. The pain continued. The pain was already in the neck, under the jaw and gave to the ear. A day later, the implant was removed. On the second day after removal of the implant, the pain went away. Now everything is calm. The picture showed that the implant rested on the nerve. I am told that the reason is in the tooth, not in the implant. Can it be?
Hello, Jasmine! In such a situation, it is usually necessary to conduct a CT examination and assess the position of the implants placed relative to the mandibular canal, since the complaints that you are voicing are really characteristic of compression (squeezing) by the mandibular nerve implant. It happens that doctors install implants close to the nerve - in your case this is a likely option, as evidenced by the pain after the removal of the implant
The adjacent tooth, most likely, was not the cause of pain, however, in order to conduct an objective assessment, it is important to see the whole picture: the results of an X-ray examination and the data obtained when examining the oral cavity.
On August 27, 2016, two implants were installed at the bottom and one at the top, but just below was one of the implants, which is under the canine, in the lower jaw. The next day, the lips began to go numb and the right side of the lower jaw, where this implant is located. And the swelling is even greater than on the first day. On August 27, 2016, baths were prescribed: baking soda with iodine in warm water, Ciprolet 500, 2 tablets per day, physio - ultrasound and magnetic, and phototherapy with a Zepter apparatus. They said that healing could last a month. The picture was taken 29.08, they said that a good picture. But swelling and numbness of the jaw does not pass. No pain, I am not complaining about the other 2 implants.
Hello! After installing the implants, this is possible, it all depends on the quality of the work performed and the body's response to traumatic intervention and foreign materials. As for numbness, it is either damage to the nerve through the nerve canal (extremely rare), or compression of exudate (hematoma, edema) of the same nerve trunk (most often). I can’t say for sure, your attending physician is more informed about this. In principle, judging by the appointments, I can’t say anything bad: more than fully.
It goes without saying that healing after implantation can be delayed for a month or more. I think that the swelling will pass faster than numbness: just a week has already passed, and most likely, it feels already significantly better. Numbness can take a long time: it all depends on the listed possible reasons for its development. Most often kept 2-3 weeks or a month, at least - up to 6-12 months. I do not know whether I was encouraged or not, I recommend to find out the details from your dentist, let him honestly explain that yes how - at least according to the pictures of the location of the implants in relation to the maxillary canal.
Good day! Today is day 6, as 6 implants were installed on the upper jaw with bone grafting (sinus lift). I have two days of bad breath. The doctor asked, he said that this was normal. Thanks in advance for the answer.
Hello! I think that an unpleasant smell is associated with a violation of hygiene because of the fear of damaging the implants. Recommendations that most often occur after implantation:
1. Adequate oral hygiene using a soft bristle toothbrush and a minimum amount of paste (2-3 times a day);
2After a meal, as well as after brushing your teeth, it is important to rinse the oral cavity with an antiseptic prescribed by a doctor or a special rinse at least 3 times a day.
The return of a proper level of hygiene after implantation will create conditions for the disappearance of an unpleasant smell. Be sure to consult with your doctor individually for the selection of oral antiseptic and rinse.
The main thing is not to consider in any case your condition after implant placement far from normal life. Just have a list of appointments and some rules that allow you to make life as comfortable as possible. Thanks for asking.
After the operation, it is really necessary to pay great attention to oral hygiene, as any food plaque on its own teeth or structures that are in the mouth can cause an unpleasant smell.
Since there are a lot of bacteria in the oral cavity, and a mild plaque is food for them, after the operation, cleaning of the teeth or dentures is recommended, despite the painful sensations. If the installed implants do not bother you, then, most likely, the reason is the low level of hygiene.
Good day! Tomorrow is recorded on the installation of the implant, but today there is a runny nose and sore throat. Can I ignore them, or first let the cold go away?
Hello Svetlana. Implant placement is an operation, and it is recommended to perform it in the period when you are completely healthy. The fact is that immunity after the operation will be reduced, and against the background of a cold, the risks of developing local complications increase. I recommend that you fully recover and only then come for an operation.
Hello, I have pus under the implant of the lower anterior tooth. She asked the doctor to remove the implant, he refused, said that this may be due to duodenal disease. Is it possible? Thank you in advance.
Hello! For me personally, such a connection is doubtful, although some diseases often lead to implant rejection, especially if the implant technique is violated. I think that the doctor’s tactics are not entirely correct. If you have the opportunity to get another consultation in the chair of the doctor who deals with implantation in your city, then it is important to do so as soon as possible.Not seeing you in the chair, now I can only assume that the treatment is not quite on the right path.
Hello, Zhazgul! In the situation described by you, removal of the implant is usually recommended, since its porous surface is already infected. However, an objective final assessment can be given only after a CT scan and subsequent examination of the oral cavity.
Of course, general somatic diseases of the whole body can affect the condition of the dental system and soft tissues of the oral cavity as a whole, but in your situation the causes of the appearance of purulent discharge are local factors, such as infection of the wound during surgical treatment or poor hygiene. It is extremely doubtful that a duodenal disease could somehow affect the situation. We strongly recommend that you contact a specialist as soon as possible.
Hello! Six years ago I had two tooth implants in my left upper jaw. For the past month, they stagger and bleed. The smell is unpleasant. Should I see a dentist? There is no implantologist in the village.To go to the city where they put, there is no possibility.
Hello! According to your description is similar to signs of rejection of implants, almost 100% - periimplantitis. Refer to the dentist is necessary to clarify the diagnosis. Unfortunately, the fact that there is no implantologist in the village may not leave another option (if you don’t go to the city), except after making a diagnosis related to rejection of implants, remove them in the village where there is a dentist-surgeon. And then - plan a trip to the city (you can even go to another specialist in the field of implantation) and put either implants, or use an alternative prosthesis (for example, to make a bridge, or another - it all depends on your situation in the mouth). If there is an orthopedic surgeon in the village, then instead of implants you can perform simple prosthetics. I do not think that you will be able to re-implant under the guarantee, although 6 years is not a long service life for high-quality modern implants.
Hello, Heaven! It is necessary to consult a dentist-surgeon for an examination.The symptoms you describe are similar to periimplantitis when the implant becomes unstable due to the attachment of an infection and atrophy of the bone tissue around it. I advise you to remove these unstable implants in the near future, so as not to aggravate the situation of loss of bone tissue. It is necessary to preserve bone tissue as much as possible. Then, after removing the implant, it is necessary to wait for its recovery and complete healing of the wound - this is at least 4-5 months. Then re-do a CT scan and assess the condition of the bone tissue. Only after that it is possible to create a new treatment plan.
Two implants on 4 teeth (left upper) sunk into the sinus, ichor, soreness. Where to find a specialist?
Hello Vladimir! Judging by the situation you are describing, inflammation is now observed in the left maxillary sinus. The reason for this, most likely, was implants - I assume that against the background of their overload there was bone resorption (loss) around the implant and subsequent inflammation. Overload occurred due to the small number of implants on a large number of chewing teeth. Patients with problems of this kind often come to our clinic.Each case is individual, and you need to study the whole picture in order to correctly diagnose and solve the problem as accurately as possible.
At the current moment, I can say that you need an implant surgeon and an orthopedist. Together they can help you.
Hello. On my 3rd day after the implantation of the two front teeth, edema appeared, the eye swelled and a bruise ... Near the implants, something white, like pus. The sky was stitched, and it was also chased. What to do? The doctor said that swelling is normal. Pricked himself intramuscularly demictasone.
I drink amoxiclav, I clean my teeth gently, I rinse chlorhexidine after eating. Swollen more left side, to the eye.
Hello! There may be swelling after implantation, but with the spread of edema you described, it does not hurt to consult a different maxillofacial surgeon to rule out possible complications. I see no point in contacting the attending physician, since his opinion is already clear - he considers the spread of edema “under the eye” to be the state of the norm. According to the information you provided, I cannot tell you anything moresince a careful examination is required in the oral cavity, a determination of the state of the tissues during palpation is possible, as X-ray control will be required.
Thanks for the answer, and for your participation to me. My edema was asleep, there were some minor bruises, they turned yellow. Inside the mouth, everything is slowly getting better. Today is 7 days after implantation, the other day I will go to remove the stitches. Thank you again, all the best!
Hello. During the implant installation, I had a hypertensive crisis, pressure 200/120. Was taken to the cardiology center. The doctor said it was a reaction to anesthesia. 2 months have passed, now the doctor is afraid to continue working with me. Advise what to do? Thank. I am hypertensive and I have atherosclerosis of 60%.
Hello Larissa! Situations of this kind are not uncommon. Against the background of a general psycho-emotional stress and the use of an anesthetic containing adrenaline, blood pressure always rises. And since you have hypertensive disease and atherosclerosis of the blood vessels as a concomitant disease, this already means that it is impossible to perform the operation only under local anesthesia. You must use sedation.
Sedation is not anesthesia, but the so-called potentiated analgesia, when special preparations are used, which are introduced into a state of slight prostration or superficial sleep (drowsiness). That is, you will remain conscious, but you will not remember the moment of the operation. In this case, you will perform the commands of the doctor, being in a relaxed state. It is comfortable for you and the doctor. After that, the joints do not hurt, the muscles do not hurt, and an operation can be performed within 3-4 hours. During the procedure, the anesthesiologist also administers an antibiotic, antihistamines and anti-inflammatory drugs. He constantly monitors your condition. At the same time, the doctor who operates is focused on surgery.
Consultation and an opinion on the authorization of the operation from a physician and cardiologist will also be necessary You may need to correct the regimen of certain drugs that you are taking.
Hello. In March, I was replaced with an implant in place of the top four. There the bone was atrophied, and I was implanted together with a sinus lift. Almost a year has passed, but now my implant is completely palpable through the skin, as if the bone is not there (this is on the front side). My doctor will be only in January.In connection with this question: is it possible to plant more bone on this side, while not touching the implant? And if you don’t touch it, will I stay without an implant? Nothing hurts while pressing. She gave a lot of money, went to the best clinic in the city, and this happened ((
Hello! I would recommend to do a dental computed tomography (VCT) in order to understand the reason for the development of this problem. Without a picture it is difficult to advise anything blindly. It can be assumed vestibular implant installation, that is, it means that the implant was oriented significantly to the outside, and the wall is thin. That is why resorption of the outer cortical plate could occur - and, as a result, the structure is now felt on palpation. It is necessary to look at the degree of bone resorption (in some cases it is better to reinstall the implant). Again, only the doctor can make a final decision after examining the situation during the examination.
Hello. I will add that if the implant is really palpable through the gum (if I understood correctly, “through the skin”),then this is an absolute indication for the operation of the implantation area revision, during which the stability of the implant, its degree of exposure and the possibility of closing it with bone material are assessed. It is not excluded that the implant will need to be removed. An audit is needed in the near future, as the situation may worsen over time - then the chances of preserving the implant will decrease.
Hello. I got an implant seven days ago. And the gum is still swollen. A little bit of a white spot like a pustus. Tell me, please, is this normal?
Hello! I do not think that your description falls under the category of norms. I recommend the following procedure: consult your doctor for advice. If the implantologist determines the problem and makes the correction of treatment, then all that remains is to wait for positive results. If the doctor assures that it is normal and does not take any action, then it is advisable to consult an independent doctor who is implanted in another clinic.I understand that in a commercial environment, sometimes not quite professional doctors begin to criticize the work of a previous expert without good reason. But in this case you will feel it necessarily. Be that as it may, without a detailed examination of the state of the surrounding gum implant, it is difficult for me to draw conclusions as to how dangerous it is. Better to be safe and get in-person advice.
Hello. I agree with my colleague. In general, the situation of purulent fistula is described, which indicates the presence of an inflammatory process around the implant. An urgent need to consult a doctor.
Hello. I was given an implant 20 days ago. Removed the seams. All is well. But today the implant became visible in the gum a little, it was not visible before. I press on him slowly - a crunch is heard. And I began to feel the implant itself. Tell me, please, what does it all mean? So it should be?
Hello. Week 3 is one of the critical moments in the process of osseointegration of the implant. Judging by the description, in your situation the implant has lost touch with the bone, has become mobile, and gradually comes out. Most likely, it will need to be removed and re-implantation planned.It is important to check the situation with a doctor as soon as possible.
Hello! Installed implants in the lower jaw. Added bone material, put the membrane, made the seams. It has been exactly one month. A few days ago I noticed some white crumbs, they are hard, they creak on teeth. Out of the hole in the gums on the side of the lower lip. Run to the doctor? Is this bone material coming out?
Hello! Judging by your description, there is reason to assume that there is a fistulous passage on the gum, through which bone material enters the oral cavity. It is too early to say that the implants have not taken root, but I recommend to contact the attending physician as soon as possible, since the situation does not apply to the normal state.
Hello. Perhaps in the area of bone grafting there is an inflammatory process, due to which the integrity of the barrier membrane has been disrupted. Therefore, the granules of bone material out into the oral cavity. It is urgent to consult a doctor to decide on the revision of the plastics zone.
I was on a visit to a doctor and asked him a question about these white crumbs. He said that everything is normal, there is excess bone material. He advised to put Solcoseryl-Dent constantly, until he healed everything. In principle, now there are almost no these crumbs.
I forgot to ask the doctor, maybe you will say: sometimes in the gum there is a pulsation in the area of the implants - is this normal?
Hello! I'm not sure that this symptom is the norm. However, the symptoms must be confirmed by inspection in the oral cavity + X-ray data. If you have a fistulous passage in the implant zone in your mouth, this alone is a matter of concern + you are talking about pulsation, which also confirms suspicions.
Hello! Tell me please. I am 29 years old. On December 2 (2 months ago) implantation was carried out in the area of 13 teeth (canine) in the upper jaw. There was swelling of the cheeks, it hurt terribly. After 5 days over the implant, on the gum, closer to the nose, a small lump appeared, which increased in size. After the doctor pierced it, i.e. a week after implantation, fluid began to run out, pain and swelling began to decline.The doctor prescribed a laser, the gums practically did not hurt, only with strong pressure, but pus slowly flowed out of the gums. They took a picture, the implant gets accustomed well, there are no blackouts, there is no pain either, but here pus appeared in a small amount when pressed on the lump and ran down the front wall of the gum and went out to the side of the implant pin, or it is not clear ...
When this bump appeared, drank antibiotics, rinsed Betodene, water-salt-soda. Plasma lifting of gums was done 2 times, pus was slightly excreted, but, of course, less than before. The cone disappeared, but the pus was coming from the side of the pin ... Before the new year, the doctor put on a plastic crown, but left room for the pus to drain (the implant itself was set a bit oblique, that is, at an angle - as the doctor explained to me, where ). Of course, I feel better, but when pressing on the gum from above, closer to the nose, a small amount of pus is still released. In the area of the crown, neither redness nor painful sensations, redness on the top of the gum, closer to the nose. The only thing - worries pus, although in small quantities.
Tell me, please, does the discharge of pus talk about periimplate? 2 months already I go with inflammation ... But when tapping the implant does not hurt, does not falter, does not bleed.What should I do in this situation? Wait, when will stop going pus? Or is it better to remove it now and try again later, but I don’t know if I will decide again ... Sorry, that’s so detailed. I would love to hear your opinion ...
Hello. This period of suppuration indicates the presence of chronic inflammation in the area of the apex of the implant. Most likely, its tip comes out of the bone in the area of the nose and is under the gum. To clarify this situation, it is necessary to do CT (computed tomography), and not OPTG (panoramic image). If so, the implant must be removed. If the top of the implant is in the bone, but there is a darkening around (according to computed tomography), then it is necessary to consider the possibility of revising the area of the top of the implant.
Hope for an independent cessation of suppuration is not worth it. I recommend to get an internal consultation in another clinic with an implantologist, who can give an independent assessment of the problem and carry out an in-depth analysis.
Hello. Two years ago, implants were placed on the upper jaw, 5 pieces, everything.Weeks two are tormented by mild aching pain, and when walking or jumping, it gives off to implants. Feeling - as if knocking on them from within. There is no redness and swelling. Consult, please, what can give such a state and whether it is connected with the beginning of the rejection? Thank.
Hello! This may well determine the beginning of the inflammatory process, so you should take pictures and consult with your doctor. While it is too early to make final conclusions, but it is worth it to be reinsured - the earlier you ask for diagnostics, the more chances you have to get out of this situation with the least losses.
Hello, Svyatoslav Gennadyevich! From November 2016, she began to prepare for implantation: she cured everything that was necessary, at the end of January the eight was removed from the bottom left, the removal was unsuccessful, the crown of the tooth broke off and the doctor drilled the root. Healed for a very long time, a sharp piece came out from the side of the tongue, the gum ached and injured. The doctor "bit him off." Ranka still not protracted. 02/17/2017 implanted, the 4th and 5th tooth at the bottom right, and the 6th and 7th left.Today is February 20, everything is calm on the right, there is no pain, no swelling. Pain on the left, I do not understand what it is from — either from implants or from an unhealed wound on the gum from “biting off” the bone. The gums in the area 6 and 7 of the implant and in the area of the remote 8 are red and swollen. Today, the doctor filed a wound at the figure eight (the white bone was visible). He says that the pain of this wound, with implants is all right. When pressing on the gums in the 6th and 7th implants is painful, there is no discharge. Implants on the right have no pain or swelling. Is the doctor right? I'm afraid of inflammation.
Hello! I think that the doctor with a high probability was right, noting the inflammatory process near the eighth tooth as the cause of the problem. When the bone tissue is exposed, even severe pains can occur - this seriously disrupts the normal healing of the hole. Therefore, the doctor did everything necessary to eliminate this problem. As for the pain in the area of newly installed implants: for 1-2 weeks, pain when pressing on the gums in many cases may well be present, and this is not considered a pathology.
How to understand the mathematical inconsistency in the article in two quotes:
“On average, implants are rejected in no more than 3-5% of all cases, and the indicators vary greatly depending on the brand of structures. For example, German or Swiss-made implants successfully take root in 97-98% of cases, and more affordable Israeli or Russian-made products — at about 95%. ”
“Practice shows that dental implants in smokers are rejected more often than in non-smokers. According to statistics, approximately 30% of patients who smoke have symptoms of rejection already observed during the first five years after the operation. ”
1. Exaggerated percentage of successful cases?
2. Exaggerated the harm of smoking and the number of unsuccessful cases in smokers?
3. 98% is the percentage of engraftment in the first 1-2 years, and 30 percent of rejections is the percentage of rejection after a long period (5-10 years)?
Hello! The percentage of successful cases is an approximate general statistic. There is also a survival rate for specific types of implants.
As for smoking, the risks are definitely increasing, especially for hard-core smokers.But it is difficult to calculate exactly how many cases are unsuccessful, as each clinic has its own ways to deal with this problem. Recently, I had a patient with implants at the reception, who for the sake of them (or rather, for the amount he gave) did not smoke for about 2 years. Then he lit up again a little - and got to me.
In general, you should not look only at the percentages: for each patient, the dentist will determine his level of risks. With the normal hands of the doctor and the adequacy of the patient (the desire to cooperate with the doctor), the probability of a successful implant engraftment will be about 98% in the first months, and this percentage will decrease insignificantly, if viewed from a perspective even a decade. Otherwise (for example, if the recommendations of the doctor are not followed, if the oral hygiene is poor, if the patient is smoking badly), the risk of complications increases by 5–10 years.
Before placing the implants in the lower jaw, the bridge of 7.5 implants in the upper jaw was dissolved. The doctor had incised the gum for a larger landing of the bridge, there was severe pain and temperature. Doctors stretched for four months while they were doing the bottom.There was a pocket in the place of the cut, and everything was rotting. But doctors blame the implant and say that it should be removed, as if it was inflamed. But he stands firm, and was not sick, but just disintegrated. After cleaning now there is a sharp pain and probably will have to remove the implant. Can I expect the doctor to correct my situation? Or I can not prove anything?
Hello! Generally speaking, in dentistry to prove the fact of the implementation of a particular manipulation can be difficult. Firstly, because in the medical documentation with high probability the doctor described everything as it should and should be according to the protocols of this type of treatment. Secondly, the procedure of disputes, including the creation of a medical commission studying the images before and after, the state of the oral cavity, etc. - business is also troublesome and paid. However, if you find a common language with a doctor, then you can always agree amicably. Otherwise, you have the right to apply complaint mechanisms to his superiors, indicating your willingness to defend your rights. But, as far as I know from the unspoken statistics of Russia, the evidence base is always difficult to collect, and during its collections, the documents in the clinic are polished to the ideal.A doctor, if it starts to smell fried, as a rule, is fired, often in hindsight. The medical organization itself finds many loopholes to hush up the situation.
After installing two implants in the upper jaw, 6 months have passed. Installed gum formers. The gums ached a bit. When screwing the abutments into one of the implants, there was pain when tightening. 10 days have passed, and when pressing on the implant, dull pain is felt in the depths. The gums around the implants ache with pressure. 2 days ago installed a removable denture on the buttons. When chewing pain is not audible, but there is sometimes nagging. Can this indicate peri-implantitis?
Hello! Symptomatic sluggish in order to say 100% about the beginning of reimplantitis. And the evidence base is always based on radiological data and examination of the gums with implants. It may be that during the “twisting” the gum was simply injured, but otherwise it should take a little time to understand whether it turned out well or not. It seems to me that the doctor could not call you to the control after 1-2 weeks (or a month) to determine the quality of implantation.In this case, let him guide you according to the treatment schedule, and you can safely tell him your concerns so that after the diagnosis, examination and analysis of the situation, conclusions are drawn and the treatment is adjusted (if necessary).
Put 2 implants down on the chewing teeth. One implant quickly settled down, and the second rocked a little, but there was no pain. Slight swelling. The doctor said that the last tooth did not catch on. Redid, again unsuccessfully - touched a nerve and there was a hematoma (half of the lips were numb and the impression that a tooth would come to a tooth). The implant was changed again, but the sensations did not change - the same dumbness and great swelling. It is impossible even to swallow, such pain when swallowing.
Put the implant 2 years ago, on the canine. Over the canine on the gums comes pus. The antibiotics has been cut, the discharge has decreased a little, the implant does not loosen and does not hurt. I want to remove it and forget about implantation, put a crown, is it possible? Thank.
Good afternoon, yes this is possible! But I recommend to be examined by a qualified specialist and find out the cause of suppuration.I would not recommend cleaning the implant, if possible. If the implant needs to be removed, it is better to do the reinstallation later. Bridges lead to major problems in the long term: to install the prosthesis, you need to grind the adjacent healthy teeth, and this is their serious and irreversible damage. In addition, if you want to remove the implant, you will need to replenish the bone tissue, otherwise the gum under the crown of the denture will quickly squeeze and the aesthetics will be broken, moreover, atrophy will lead to mobility of adjacent teeth, and the whole structure will not last long.
My opinion: the installation of a dental bridge instead of an implant to replace 1 tooth in this situation is inexpedient neither from the point of view of treatment effectiveness, nor from the financial side. But it's up to you, of course. I only insist on not drinking antibiotics without an appointment. It is necessary to identify the cause of suppuration in the area of the implant with an experienced specialist and, if possible, save the work done.
Many thanks for the advice. It was the other doctors, the problem is not in the implant, it is near the tooth, which is wearing a crown, inflamed. We treat.
Hello. 5 days ago put the system "all on six implants." Until the prosthesis was installed, the pain was weak, the edema was, of course, severe, but there were no bruises. Two days ago, "screwed" prosthesis. Now the constant aching pain, much receding in the ears. I do not live without pills. It seems that the doctor has tightened the screws. In the process, I told him that it hurt, but he said that he must pass. However, it does not pass. He was on vacation, did not pick up the phone before leaving, although he called more than once. Shoots in the ears, pressing in the jaw-arching pain. But more worried about the ears and throat, as it is not strange. There is no smell, but the sensations are very similar to a toothache, and the whole jaw hurts. What is it?
A targeted shot of the two implants was made during the installation of the prosthesis. Can there be pain from too tight swirling joints between the implant and the prosthetic nuts? The edema is almost gone, but there is a strange and painful seal in the front lip. Antibiotic drink, rinse after each meal. Honestly trying to clean, but very painful!
And yet, the prosthesis was installed on the third day after the operation, without removing the sutures, and the jaw was literally screwed tight on the barely alive after removal of the implantation, suturing and other related pleasure.
Ears and throats are very sore. Why?
And the second.In drawing up a treatment plan, the doctor suggested Adi's implants at the appropriate price, and put the MEDENT. But for some reason I have not voiced it. And they are much cheaper, IMHO? Is it worth arguing? And is there a chance to achieve the truth?
I'm worried about your complications in the ears and throat. As I understand it, the prosthesis took place on the upper jaw. If the Zygoma type zygoma implants were used as part of the All-on-6 complex, then it is likely that the implants in the sinus area were not installed correctly. As for the implants of the firm Medent - I am not familiar with them. Adin implants are known, but in our clinic we do not use them for a number of reasons.
An aim picture is not enough to understand the picture, you need to do a CT scan. You can send a picture to the mail of the site, I will comment. Also, if you wish, you can sign up for a free consultation with me.
Regarding the brand of installed implants - of course, it is worth arguing, since you had to install exactly the brand of implants for which you paid. All data must be specified in the contract.
Thanks for the answer. I implanted the bottom) It took 7 days, all appointments were made, and the pain (especially night) remained.Today I thought I would live without a pill, but I realized that the gingival body itself, on which the prosthesis is installed, is very painful and shoots at the bone so that it is not clear - is it ear, throat or implants? .. Anyway, it’s like a fresh stump of the arm, example, put on a prosthetic arm. In the ear shoots. If she could, she would have removed the prosthesis. Very painful!
This is normal? I was at the reception in this dentistry - my doctor was on vacation, so another doctor looked at me. She said everything is fine 🙂
I do not live without ketanova! Interestingly, you have to drink it all your life? I was not warned about this ((
Good day! If implantation is performed on the lower jaw, then the symptoms of pain are similar to trigeminal neuralgia. As I already wrote to you, I highly recommend doing a CT scan in an independent laboratory. The results of CT in the event of further clarification will help you a lot.
If the nerve is damaged is not critical, then over time the pain can go away on their own.
Do you have any numbness or feeling of anesthesia?
No, there is no numbness. I understand that because the body of the gum hurts, everything starts to hurt. Or I don’t understand anything that hurts me 🙁
Yesterday I contacted the doctor from the clinic where I was operated on, said to take diclofenac and miramistin. Miramistin replaced chlorhexidine, diclofenac drink. Today, I'll come to see me. I do not know when these pains will end ...
Good day! I have adentia of the upper jaw, many teeth were removed 15 years ago, for more than 5 years I have been wearing a full removable denture. A recent CT scan shows bone failure all over the upper jaw, as the surgeon said (I don’t know how much is left). I really want to do implantation, but there is a “bunch” of diseases, including: chronic glomerulonephritis (kidney function preserved, experience of 35 years), hypertension of 1 degree, stage 2, risk 3, tachycardia, carotid arteriosclerosis, stenosis of the left carotid artery 40%, hypercholesteremia, multinodular goiter, euteriosis, osteopenia, vitamin D deficiency, etc. Thyroid hormones are normal. I constantly take calcium channel blockers and statins. I am 46 years old. I ask you to answer the question: with such a “bouquet” of diagnoses is it possible to perform implantation (the general practitioner concluded that there are no contraindications).And is there any hope that the implants will take root? And is it possible to count not on a removable prosthesis on implants, but on a nice bridge? Thank you in advance!
I forgot to point out that I am still allergic ((Glucosamines, some vitamins, food allergies.
Good day! You may come up with one of the most low-impact methods of implantation with the immediate load of the Basal Complex, or otherwise, the basal implantation of teeth. If your therapist reports that there are no contraindications, then implantation can be performed. But first, I need to familiarize myself with computed tomography (CT) and the state of the oral cavity. And also study your medical history in more detail.
It is important to choose the right method of anesthesia in your case. You can probably calculate the “nice bridge”, the prosthesis is fixed for 2-3 days after implantation, and you can start using new teeth almost immediately, gradually increasing the chewing load.
If you wish, you can sign up for a free consultation with me. If you do not have a CT scan, you can do it at the clinic. Capture, please, the conclusion of the therapist.
Good day. Tell me, please, the situation is as follows: 4 days ago they put implants on the left side, 2 upper 1 lower ones. After the operation, there were no serious symptoms for several days. But she began to notice that from below a nearby, a living tooth began to ache when pressed and stagger a little. And today, the nose is stuffed up on the same side where the implants are, and when blowing your nose, there are dense snot with blood.
This is the norm, or urgently need to go to the doctor? At the reception for the removal of stitches to me only after 1.5 weeks.
Good day! In any case, you need to urgently go to the doctor and take a control picture, to understand the nature of the mobility of the adjacent tooth in the lower jaw.
“Blood snot” is, of course, a suspicious symptom, but it may not be of a dental nature, especially if you haven’t had a sinus lift and implants are installed outside the maxillary sinus.
Hello. Please explain why, after installing the gingiva former on a normally implanted implant, did inflammation occur? When the doctor screwed it in, I felt pain as it penetrated deeper. Maybe this is the wrong gum shaper?
Good afternoon, inflammation could occur due to soft tissue damage and microbial invasion during the installation process of the gum conditioner. It may be worth unscrewing the shaper and reorganizing the area, reinserting the implant plug and waiting for tissue rehabilitation, and then going through the shaper installation stage again. If the shaper was “not native” (from another system of implants), then during its installation damage to the implant in the bone could occur - for example, different threads in the internal cavity of the implant and strong pressure of the doctor when trying to screw the shaper. This could also entail an inflammatory process.
Need to look at the picture and the area of inflammation. If there is an opportunity, you can sign up for a free consultation with me, I will look and tell more precisely the reason and what to do next.
The day after implantation, swelling, pain, and subfebrile fever appeared. I began to rinse with salt and soda, drink ibuprofen and an antibiotic. We have 3 days off, so I could not see the doctor. Is it possible to install crowns on such an implant? And why did inflammation occur?
Good day! It is impossible to install the crown immediately after the implant is implanted by a two-step protocol. The fact that edema appeared immediately after installation is quite normal, but a rise in temperature above 37 is a bad sign. Perhaps for some reason there was inflammation around the implant - you definitely need to see a doctor. The measures taken by you, in my opinion, are fully justified for the weekend, but even if the inflammatory process is stopped, the doctor still needs to appear, having reported his problem.
After the implant is fully engraved, the crown will be installed, and the new tooth will serve you as your own. The presence of the inflammatory process (in time stopped) does not at all indicate a negative outcome of the entire implantation.
Hello! After removal of the 4th upper tooth (with a cyst), an implant was immediately placed (Nobel) ... The implant was not sick at all, but after 2 months inflammation developed away from the implant, and often there was aching pain in the bone at one point, periodically swollen , the gums on the 1st, 2nd and 3rd teeth were inflamed.The doctor claimed that everything was fine and that he could not see anything.
I did a CT scan, at which the doctor also did not find anything, however, he said that if he continued to be ill, he would have to remove the implant. When he began to remove, the implant fell out easily, i.e. did not intend to take root from the very beginning. It would seem that the inflammation was removed and the cause was established, but the pain in that same place remained, and the entire gum in the area of healthy teeth still periodically swells up. The doctor is extremely annoyed and believes that I am inventing. Please comment on the situation.
Good day! 4 the tooth is in the zone of the maxillary sinus, inflammation may occur if you have problems in it. You write that the doctor watched a CT scan, but did not find anything, while, judging by your impressions, the implant did not catch on. It all looks pretty weird. Nobel implants (original) - very high-quality products, and when properly installed, the percentage of their rejection is almost zero. Those. On poor-quality implants in this case it is not worth sinning.
The following possible reasons remain:
1. Infection when a cyst is removed has spread to adjacent areas in the bone tissue (it cannot swell up without an inflammatory process);
2When installing a dental implant, there was damage to the periodontal tissues of the neighboring teeth - sometimes doctors screw the implant slightly at an angle, and here it is important to ensure that the artificial root does not damage the tissue of the adjacent living teeth.
3. Or you have inflammation in the maxillary sinus, which gives complications.
Hello. Recently, I removed three teeth, I want to install implants now. I read on the Internet about various firms - they write that some implants can take root in different ways because of the different coverage. Is it so? Does anything else affect the engraftment of implants from different companies? I would like to know the opinion of experts. Thanks in advance for the answer.
Good day, first of all, the survival rate of the implant depends on the qualifications of the doctor and on how the patient complies with all appointments and instructions after implantation. Regarding implant brands - yes, indeed, there are differences. My opinion: you need to choose time-tested implant systems, for example, Nobel Biocare, Straumann, Xive, AstraTech, Bio Horizons - they fall into the premium category. From the budget category, I would recommend MIS, Osstem, Simpl Swiss.
“They write that some implants can take root because of different coverage” - quite right, that is why implantologists usually work with several implant systems, and not only for financial reasons, but also because (in particular, an important indicator - the state of bone tissue) are different requirements for the thread, shape and type of implant installation.
Hello! Tell me, please, if the zygomatic implants do not survive, then they are twisted back? Thank.
Good afternoon, yes, in this case there will be a reinstallation of the zygomatic implant with a wider thread in the same bed, or the penetration vector may slightly change according to indications.
Hello! Installed the implant two months ago. They immediately made a plastic crown. After the installation, there were almost no discomfort, but antibiotics were drunk by prescription. Now I got pregnant, the implant does not bother, there is no pain. But the redness around the implant does not pass and lasts all 2 months.The doctor said that a reaction to a plastic crown is possible. Tell me, please, is this possible? And how can I be on the assumption that I'm pregnant?
Good afternoon, yes, indeed your doctor is right, there may be an allergic reaction to the plastic. Since 2 months have passed, you can change the crown to a permanent one. But first you should take it off, watch the reaction of the gums and make sure that everything is fine with the implant. You didn’t write what implant system was put to you - some systems achieve stabilization in 2-3 months, and you can already install a crown of zirconia or metal ceramics.
Important note: all these manipulations can be performed after the 1st trimester and under the strict supervision of your gynecologist. Much depends on your condition during this period. If the pregnancy is difficult, I recommend not to resort to prosthetics, but simply to remove the crown and gently care for the implant.
Good day. Yesterday, we installed two upper implants, one of which was in the hole from the newly extracted tooth. I had to pay 10 thousand for the material for building bone, becausethe hole was wider than the implant itself. At night, I woke up from the sound of a crunch in the place of the implant installation. I drink antibiotics, the pain is gone. The crunch was not repeated. Do I need to be afraid of this sound and run to my doctor?
Good afternoon, people often grit their teeth when sleeping (for some, even this is a disease called bruxism). The crunch, most likely, arose due to excessive stress on the implant and artificial bone. I highly recommend that you consult a doctor and take a control shot.
Recently, an implant fell, put 7 years ago. What do you think, what could be the reason? For hygiene always carefully watch. I think it's not about the implant itself, because for seven years there were no problems.
Good afternoon, Elizabeth. It is difficult to answer your question without conducting an inspection of the oral cavity and not having pictures in your hands. Perhaps, an error was made when inserting a tooth into the jaw row at the stage of prosthetics. The crown should be precisely selected on the bite, that is, fit snugly to the opposite teeth (to be in contact), both at rest and when chewing. This ensures uniform distribution of the load on the implant.If the orthopedic construction (crown) is incorrectly made and installed, the implant can be overloaded, which can lead to its destabilization.
It is also possible that there are some more serious reasons - for example, a disease of the bone tissue (the process of dilution led to the loss of stability of the implant). There may be many options. If you send a snapshot (to the mail of the site), I could analyze it and comment on it in more detail.
Good day! On November 15, an 8th tooth was removed on the upper jaw. They were prescribed to drink the antibiotic flemoxin solutab, 250 mg, taken one 2 times a day for 5 days.
After that (November 23), she installed implants in the upper left jaw: 5 and 6. Slightly increased the bone from above, sewed up and immediately installed the gingiva former, put dentium implants, appointed to treat chlorhexidine and smear metrogil dent, and if there is pain, then take 1 tablet of arcoxia once a day. Antibiotics have not been prescribed since I took them recently.
It is now the third day after implantation, and only on the third day small edemas appeared (the gum was swollen from the very beginning).The pain is the same aching. When treating metrogil dent, there was some blood, but it soon passed.
I have a question: is everything OK with me, and should I start taking antibiotics?
Hello Olga. Edemas often increase by the third day, and this is normal. The pain can persist for up to 3 days, then if the pain does not go away (does not decrease), you should coordinate the possibility of resuming antibiotics with your doctor to avoid the development of infection and speed up the regeneration processes after surgery. Also, be sure to follow all recommendations and continue to see a surgeon-implantologist on a regular basis.
I was placed 4 implants on the upper jaw along with the installation of bone tissue (as it was not enough). More than 2 weeks have passed. The tumor and the bruises are gone, but I am worried about numbness under my nose. The doctor said it would pass. The seams have not yet been removed. What advise me?
Hello, Catherine. It is necessary to control this situation with the help of computed tomography, as well as to undergo examination by an implant surgeon and make sure that the implants are installed correctly and the nerve is not damaged.If everything is done correctly, the sensitivity will soon return. Perhaps there is a slight compression on the periphery tissues - this can also cause numbness of certain parts of the face.
Good day! After the installation of 2 implants and sinus lifting in the upper jaw, a month passed. Cheek edema (noticeable) stayed for three weeks, but there was no pain. Now the seal on the gum is very dense, but painless along the entire length of the implantation. Implanted 3 and 7 tooth. Could this be an offset bone material? The doctor took a picture and said that everything is normal, it is a dense swelling. One week after implantation, the submandibular lymph node became inflamed, the antibiotic cyran was cut through - everything went away. My age is 57 years old.
Hello, Nina Nikolaevna. Continue to observe, the prognosis of your treatment in the absence of pain syndrome is favorable. And about the displacement of bone material - here you can answer only if you have a computer tomography. According to your report, the doctor has already done this. Edema slept - this is a good sign, the tissues can actually be compacted, and then the edema resolves.
Thank you, Bulat!
Swing implant after 10 years. The most expensive German set at that time. Pain when biting. Do you have to change everything?
Hello, Alla. Biting pain is a bad symptom, there is a possibility that it is periimplantitis. In this case, the implant is removed, an operation is performed to restore the bone tissue, after which you can re-implant. But it should be borne in mind that the situation may be connected with the prosthesis - it is possible that the screw that fastens the implant with the crown is loosened, and now it causes pain when biting. In this case, the screw can be relatively easy to reinstall. Be that as it may, in any case, an examination by an implant surgeon and an orthopedic surgeon with additional control over the image is necessary.
Hello! 03/20/18 installed the implant, 4-ka on top. On day 3, she seemed to the doctor, everything was fine. A day later, her cheek was swollen (swelling almost to the eye, and very dense at the level of the nose). I went to the doctor, according to the doctor, the 5th tooth became inflamed (when you touch it, pain occurs). Made cuts, squeezed out pus. He prescribed antibiotics: Flemoxin Solutab, 500 mg (2 times a day) + rinse your mouth with soda solution.The next day, all unchanged, dense, painful induration in the cheek as it was, and remained. Tomorrow to remove the gum and seams. My worries about edema, he does not leave. What do you advise?
Hello. The occurrence of purulent inflammation in the area of implantation is always a risk that the implant does not take root. In most clinics, even before the operation, the oral cavity is reorganized (dental treatment) in order to minimize the risk of such a situation as you have.
Since the abscess was opened, and adequate therapy was prescribed, one can expect that the edema will disappear in a few days (do not worry that the edema has not disappeared the next day - the resorption process can take up to a week). However, even in spite of this, it is important to completely treat the 5th tooth so that the implantation zone does not get infected further.
Hello. An implant was placed on my lower jaw, it settled down and a gum former was placed on me. There is no way to finish the operation. Today I noticed blood when rinsing my mouth (from the place where the implant was). Tell me, can it be a rejection?
Hello, Alina! Minor bleeding is possible if the wound is still fresh and 2-3 days have passed after the shaper was installed. However, if the shaper is installed more than 3 days ago, the resulting bleeding is alarming - in this case, it is important to quickly come to the doctor for examination where the implant was placed (you may need to reinstall the shaper). It is premature to speak about implant rejection of only minor bleeding.
Good day! 2 months ago, the implant was placed in place of the sixth tooth, on the lower jaw. After implantation, nothing hurt, but I took all the preparations regularly. I have not yet installed either the gum former or the crown. A week ago, a purulent spot appeared in the area of the 8th tooth, on the same side where the implant was installed (on the lower jaw). I do not have the eighth tooth and it did not exist at all. The area where the implant is installed is not sore or red. Tell me, please, purulent formation can be associated with poor-quality implantation?
Hello, Anastasia! The cause of purulent formation in the area of the 8th tooth may be, for example, chronic inflammation in the area of the roots of the 7th tooth.To clarify the situation, I recommend to contact a dentist-surgeon and make a computerized tomography of this area for an accurate diagnosis.
Hello. Three years ago, I installed an implant. Everything stuck perfectly, the only thing that after the installation of the crown in this area ached for about 1 month. And then all the time while the crown was standing, there was a feeling that food was constantly falling between the crown and the gum. I couldn’t clean it out, since the implant is deep - I simply did not get the floss.
After 3 years in the place of installation of the implant (lateral incisor) there was a constant aching pain. The gum is fine, although it slightly raised above the crown from the side of the sky (the abutment became bare for a couple of mm). When pressing the pain does not increase. Pus, odor, etc. not. On the panoramic picture and CT all is well (as the doctors say).
The doctor removed the crown, unscrewed the abutment and installed the former (to see what happens). After that, for 2 weeks in the place of the implant (or gum) there were very severe pain. Gradually, the pain decreased, but is constantly present. Tell me, please, what to do? Doctors propose to remove the shaper so that the gum is overgrown, and then we'll see. The option to remove the implant is not considered. I suffer for 5 months.
Hello, Alexander. There may be several causes of pain in the area of the implant, and first of all it is necessary to carry out a differential diagnosis - to determine what causes the pain of the entire installed implant complex. If the cause of the pain is an implant, then, unfortunately, it is necessary to take steps to remove it. However, in most cases, the implant can be maintained with timely treatment. I recommend that you go to another implantologist (not to the one that you have already examined, and it’s better from another clinic) - for independent diagnosis and decision-making on further treatment.
Hello! A month ago, I installed 2 implants on top. When biting and tapping on implants, it does not hurt, but when you press on the gum it hurts. What could it be?
Hello, Oksana. Pain in the gums may be, for example, a consequence of the inflammatory process. Here it is worth considering what way implants are conducted - if the gum former is already installed, then there is a risk that small particles of food fall between it and the gum, as a result a pocket is formed.In this case, it is necessary to pass the examination as soon as possible with the doctor (in the future it will be necessary to improve hygiene). In general, I can say that postoperative observation is one of the most important components of the treatment process. Your doctor should regularly monitor the condition of the implants, and if any problems appear, then take steps to resolve them.
Hello. 8 months after implantation. After complete edentulousness, the prosthesis was installed in the upper jaw using the technology all over. One of the implants, just to the left of the nose, pulses. I turned to a doctor, took a picture several times - everything is normal in the picture, there are no inflammations around. They made a prosthesis freely, so as not to put pressure on the gum - it did not help. They say that everything is fine with you, but the pulsation is as it was, it is. And this is not gum, the pulsation was always after installation, it was just always hoping that it would pass. How to be?
Thanks in advance for your reply.
Hello, Vladimir. Complaints about the feeling of pulsation in the area of the implant 8 months after installation - this is a great rarity. If a complete diagnosis was carried out and the measures taken by the doctor did not help,then, to clarify the situation, you can try to additionally contact another 1-2 independent specialists (preferably from another clinic). If not one doctor was already addressed, and no one was able to provide assistance, then only one obvious option remains - removal of the implant with subsequent reinstallation.
Three days ago, we removed three teeth in the lower jaw on the right and immediately put in implants (it turned out through one tooth). I take anticoagulants and said this (more than once) to both the dentist and implantologist. Edema gradually subsides, but a large hematoma with swelling of the lips does not pass. I do all the hygienic procedures and take the drugs rigorously. The swollen lip is slightly bloody, as it comes into contact with the tails of the sewing material, and I feel a lot of tails. The husband installed the implants several years ago and the sewing material was self-absorbable. I sewed, in appearance - thin fishing line.
What should I do besides the prescription of a doctor for hygiene and laying Solcoseryl Dent so that the hematoma resolves? She looks dark, like a birthmark, and under it is thick fabric. My doctor thinks it's not scary.It is impossible to lay Solkoseril between the lip and the jaw, they are in the same plane. I'm afraid of tissue necrosis.
Hello, Vera! In the postoperative period, a hematoma can indeed form in the area of surgery - especially since you are taking anticoagulants. So this is a kind of norm option. At the moment, you need to strictly follow the recommendations of the doctor and conduct regular monitoring. In the recommendations of the doctor should be indicated anti-inflammatory, antihistamine and antibacterial drugs.
As for the applications of Solcoseryl Dent gel, they are used to accelerate wound healing, but they do not remove the hematoma by themselves.
In order to avoid unwanted complications, the doctor should carefully monitor the healing process and the safety of the seams. Normally, the hematoma will disappear on its own, and the main thing here is not to try to accelerate this process by self-treatment.
Hello. 8 months ago, an astrotech implant was placed on the front tooth. Caught on. A month ago, the gum former was placed - the gum was pressed very tightly, painfully, and the crown was hitched. For a month nothing bothered, nothing hurt, and suddenly a pustule appeared over the gum.
Why could it happen when forming a gum and having a temporary crown, because the implant was placed 8 months ago? Is it really a rejection? For a whole month nothing manifested itself, it did not hurt, but here there was a small abscess. It turns out that I went for a month with internal inflammation? Very worried about the implant.
Hello, Lily. It is unlikely that this fistula is due to the inflammatory process around the implant - most likely, the infection accumulates under the temporary crown, which led to inflammation of the gums. In such cases, the crown is usually removed and the junction of the crown and the implant is treated. In any case, you need a medical examination to clarify the true cause of the problem.
Good day. I went to the doctor then, the crown was removed - everyone rinsed. They said that the gum was a little inflamed, everything was fine with the implant, perhaps food had entered. The abscess after did not jump out. Went on vacation - and here again jumped out. But in connection with the vacation I can get to the doctor only in a week. Tell me, if food has fallen under the temporary crown and the gum has become inflamed again before the formation of the dagger,so what will happen to the permanent crown? Will the food also fall under the gum? Will I always be tied to the dentist? Do I need to take a picture just in case? I am very worried because I have experienced more than one operation in the gum area. It is very disturbing that all this started after the installation of a temporary crown.