Next you will find out:
- Is there a dental implantation for periodontitis, and what difficulties may be observed in this case;
- What exactly happens in the oral cavity during periodontitis and periodontal disease and how these processes affect the success of the implantation procedure;
- What are the options for prosthetics depending on different clinical situations;
- What types of implants can be applied in case the patient has periodontitis (periodontal disease);
- What is important to pay attention after the implantation of teeth already at home, in order to prevent periodontitis to continue its destructive work.
Periodontitis today is almost the same common disease as caries, and often leads to mobility and multiple extraction of teeth. The question of whether it is possible to put implants in periodontitis, has matured from the very moment when the technology of dental implants has just received its scientific justification and gradually began to gain popularity.Doubts about the feasibility of implantation of doctors have arisen in relation to such diseases as periodontal disease (which occurs in approximately 1-3% of patients).


Generally speaking, dentists are divided into two camps: some believe that dental implants for periodontitis and periodontal disease is a very dubious event. However, others, on the contrary, note the high efficiency of prosthetics on implants even in the presence of these diseases.
At the same time, the approach to the problem is of particular interest. For example, maxillofacial surgeons and implantologists consider it a waste of time and money to “strengthen” hopeless teeth on the background of periodontitis and even more so on periodontal disease, while periodontologists introduce the latest developments related to the preservation of teeth from the removal of these diseases and they strongly advocate the fact that such teeth should still be saved.
On a note
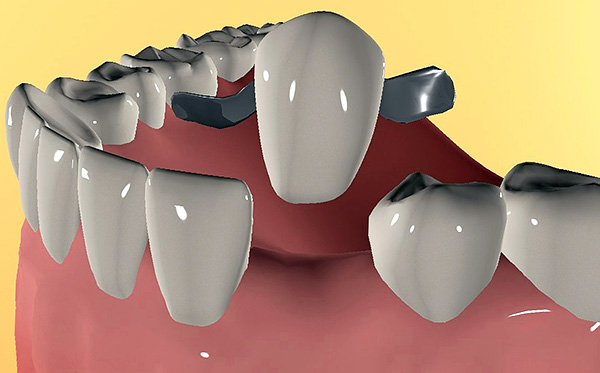
Dental implantation is an innovative prosthetic technique that allows replacing lost or problematic teeth by implanting metal “roots” in the jaw with subsequent fixation of crowns on them.Such crowns on implants allow not only to imitate natural teeth in aesthetic terms, but also to restore the lost function (chewing) with the restoration of a full bite.

So is it possible to put implants for periodontal disease and periodontitis, and in what cases to prefer this approach? In order to better understand the specifics of the problems and difficulties that may arise, let us first understand what exactly happens during periodontitis and periodontal disease with the tissues surrounding the tooth ...
What happens in the mouth with periodontitis and periodontal disease
The predecessor of periodontitis is most often gingivitis, an inflammation of the gums that occurs without compromising the integrity of the periodontal junction. Gingivitis can appear in childhood and adolescence due to the accumulation of bacterial plaque on the teeth against the background of improper orthodontic treatment, stress, smoking, immune disorders, acute and chronic diseases, malnutrition, malocclusion, poor oral hygiene, lack of adequate dental treatment, and t .d Bacteria (less often fungi and viruses) become the direct cause of the onset of inflammatory processes in the gums, which sooner or later turn into periodontitis.

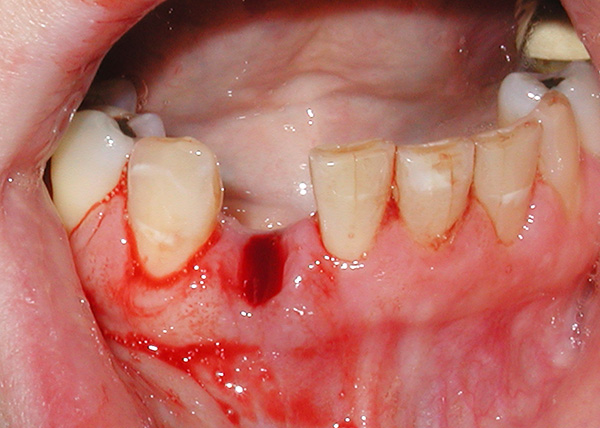
Periodontitis is one of the most frequent causes of tooth loss, since as a result of disease progression, there is literally the destruction of the dental “cells” in which the tooth is held. In the initial stages, the symptoms of periodontitis are minor: against the background of abundant dental deposits (stone, plaque), gums bleed, sometimes even a small mobility of the teeth can be observed.
But exacerbations of the disease are extremely painful in terms of symptoms and the psychological state of a person: in addition to severe bleeding from the gums, there starts suppuration from the dental pockets, strong mobility of the teeth with dislocations, pain and burning in the gums, bad breath and an active loss of jaw bone tissue . All this in aggregate, in fact, can create certain problems for the implementation of dental implantation.

Unlike periodontitis, periodontal disease is not an inflammatory disease. Therefore, with periodontal disease, there are no gingival pockets, suppuration and mobility of the teeth, but against the background of their good fixation, the necks of the teeth are exposed with progressive bone loss. Reducing the height of the interdental septa on the background of foci of osteoporosis often leads to tooth extraction, and since periodontal disease is not a local, but a generalized disease, almost all teeth that have lost bone support are removed.
It is interesting
A number of dentists (mainly maxillofacial surgeons) believe that a disease such as periodontal disease does not exist at all, preferring to allocate only periodontitis as an extreme form of gum inflammation, leading to loss of teeth. However, supporters of the traditional approach do not want to recognize their views as obsolete and until now in dental practice they use the ICD-10 working classification of diseases, where periodontal disease is indicated by the code K05.4, and chronic periodontitis is referred to as K05.3.
So is it possible to put implants for such problems with the gums?
It would seem that the implantation of teeth during periodontitis or periodontal disease against the background of impaired tooth-attaching and loosening of the teeth can be a real help not only in restoring the dentition, but also in preventing further bone destruction (the load on the bone tissue prevents its loss).
Let's look at the most common clinical situations:
- All teeth against periodontitis should be removed;
- A significant part of the teeth with periodontitis can still be saved;
- The patient has generalized periodontal disease.
Situation 1: all teeth on the background of periodontitis to be removed
In fact, the first situation, despite its tragedy, is still a fairly common reason for patients to go to the dentist. The fact is that Soviet dentistry at one time formed in many people a strong fear of dentists, and the approach to the treatment of periodontitis left much to be desired. Therefore, until now, people of 45-60 years are turning to dentists with signs of the most severe periodontitis, when it is already impossible to save the remaining movable teeth.

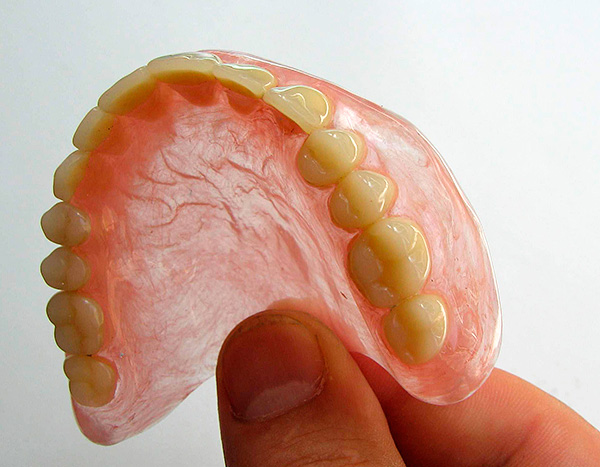
After cleansing the oral cavity of hopeless teeth in a person, there are only two ways: either wear removable dentures or perform prosthetics on implants.
The variant with full removable dentures, of course, is many times cheaper than dental implants, but it should be remembered that removable dentures are characterized by certain disadvantages:
- They do not stop the atrophy of the jaw bone tissue, and in some cases even aggravate this process;
- The second drawback is a long period of getting used to removable dentures;
- In addition, in 60-70% of cases, removable dentures do not satisfy either aesthetic or functional parameters (in other words, they do not color the person very much and are not very comfortable to wear and chew).
As a result, to date, most dentists tend to argue that the installation of dental implants for periodontitis is the only correct and promising solution, especially with the complete loss of teeth.
Moreover, there is a scientific substantiation of this approach: own teeth in the mouth are connected with the bone of the alveoli through the ligamentous apparatus of the tooth (periodontal tissue). It is in the ligament apparatus that there is an infection leading to a progressive loss of bone tissue in periodontitis. After removing all the teeth together with the infected ligamentous apparatus, the osseointegration of the implant, that is, its accretion with the jaw bone, will take place fully, and due to the chewing load, further loss of bone will be prevented.


Situation 2: a significant part of the teeth with periodontitis can still be saved
Consider the second case, when most of the teeth with periodontitis can still be saved. Here everything is not so clear. The fact is that long before implantation in dentistry there were a lot of developments regarding the strengthening of mobile teeth - for example, their splinting.
The classic version of that time was associated with the technique of “binding” the teeth to each other with soldered crowns. Understanding this tactic is easy: a group of mobile teeth gathered together, turning into a single whole, which made them more resistant to mechanical stress, and for a longer period of time. Currently, popular variants of splinting teeth are their “binding” with the help of aramid yarn and fiberglass.

Therefore, if all teeth (or almost all) are preserved in the oral cavity with the initial form of periodontitis, it is possible to conduct a comprehensive treatment of periodontal tissues with the use of modern devices (ultrasound, laser, etc.) and the latest technologies.
On a note
However, it should be remembered that periodontitis, according to modern scientists, is an incurable disease, although it can be translated into stable remission with the preservation of their teeth for many years. However, for this, especially in advanced cases, it will take a lot of time and money to carry out complex manipulations at the dentist-periodontist with constant monitoring (2-4 times a month) and corrections for the indications of the periodontal treatment.
If the gum treatment becomes ineffective for any reason, then the removal of the teeth is performed, requiring immediate replacement of the defect. The danger of leaving the resulting "gap" between the teeth is that the teeth left without their neighbors against the background of chronic periodontitis slowly but surely begin to "part", which leads to a violation of bite and multiple loss of the remaining teeth in a short time.
Here it is necessary to correctly determine the plan for the restoration of the dentition, without delaying this matter for a long time. But here is what is better to choose with regard to the existing periodontitis: put ordinary “bridges” (prostheses), or do spend more expensive prosthetics onimplants?
Of course, the further plan of the treatment that is appropriate in each particular case is chosen by the doctor strictly individually. However, it is worth remembering that in the severe stage of periodontitis, even after a long course of treatment, there remain serious risks of impaired periodontal attachment in the area of those teeth that the dentist can take under the bridge (there are a lot of such cases).
Every year, from 30 to 40% of cases of tooth loss are recorded along with “bridges” within 1-2 years after prosthetics. That is, there is no absolute guarantee that after the intervention of a periodontist and a course of treatment lasting from 2-3 months to 1-2 years, the destruction of the jaw bone will not continue further. The loss of bone in the future involves serious problems, ranging from multiple tooth extraction and ending with additional difficulties in prosthetics and implantation.
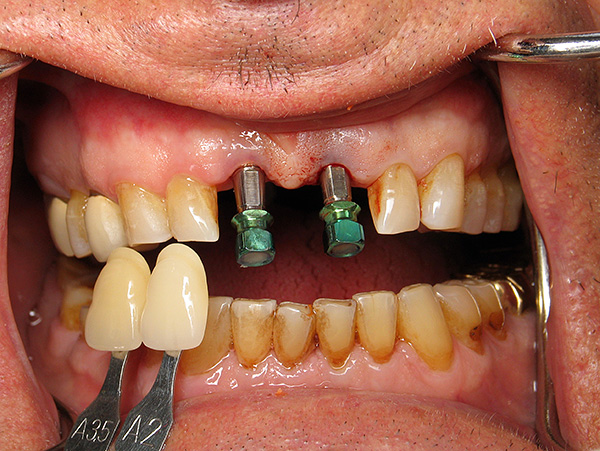
Therefore, dentists adhere to a reasonable tactic of choice: if there is an initial stage of periodontitis, then conduct a comprehensive anti-bacterial and anti-inflammatory therapy with respect to reliable teeth, and in place of missing teeth are installed implants.The main rule here is that there should be no teeth near the installed implants that have pathological gum pockets with pus and infection, otherwise the success of the implantation will be questionable.
If the doctor is not sure about the perspective of the teeth on the background of severe periodontitis, then all the untreated teeth are removed and implants are placed instead.

Feedback
“Recently I decided to install two implants below and above. About 3 years ago, before that, one tooth was pulled out from behind a cyst that burst and came out with pus, and the other tooth was simply ruined by the doctors. He was treated and healed many times to such an extent that the gums between the teeth began to swell and bleed when cleaning and even when biting an apple. At one point, he cracked at me so that he burst under the gum. In the end, I, too, tore him with tears in his eyes.
When the dentist-surgeon looked at me, she discovered that, near my last problematic tooth, periodontitis had arisen due to the constant ingestion of food in the gap, but not on all teeth. Therefore, my gums were so painful and bleeding, and I constantly felt sorry for them to clean them like a fool, so as not to ruin the wounds ... ”
Anastasia, Moscow
Situation 3: the patient has generalized periodontal disease
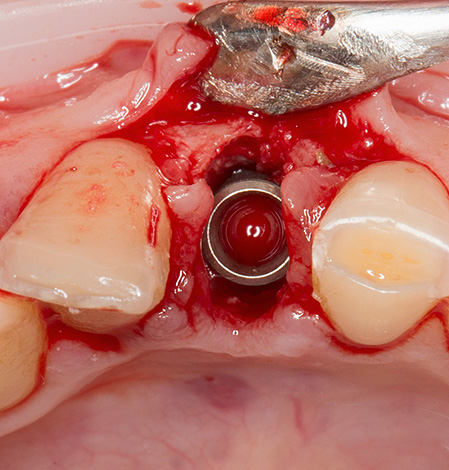
Clinical cases in which periodontal disease is diagnosed are fairly simple in terms of treatment planning. The fact is that periodontal disease is a disease that almost always leads to tooth loss. It is especially difficult for a person to have a moment of exposure of the necks of the teeth with progressive loss of bone tissue of the alveoli. Therefore, the most appropriate treatment strategy for periodontal disease is the removal of teeth and the installation (preferably single-stage) of implants.

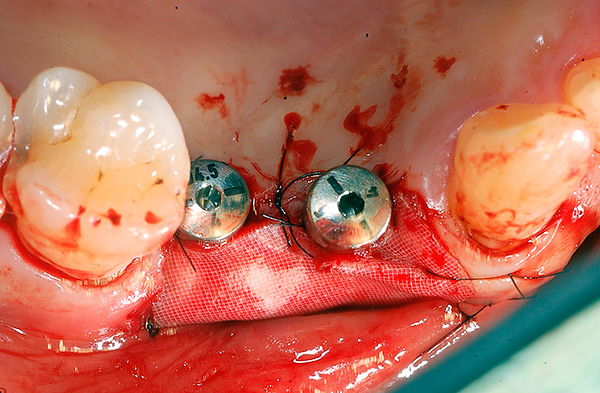
Since periodontal disease does not have an inflammatory process, there is no need to specifically prepare the oral cavity for implantation, therefore most implantologists adhere to the tactics of tooth extraction and implant placement at one time. Thus it is possible to stop the progressive destruction of bone tissue due to the return of the usual load. Sometimes in severe cases, you have to first restore the lost bone (sinus lift), and only then - implantation.
Partial and complete removable prosthetics without implantation for periodontal disease does not stop the processes of atrophy of the alveolar process, and often even aggravates them.
On a note
The surface of the installed implant is such that after “merging” it with the bone tissue, the structure becomes stronger than in the case of the native tooth. With the right choice of the implant system and compliance with the implantation technology, even with periodontitis and periodontal disease, the installed implants can fully serve up to 25 years or more.
An important nuance taking into account the individual characteristics of the state of the bone tissue of the alveolar processes of the jaw is the number of implants installed, which should ensure the optimal load on the bone tissue to prevent its further atrophy. Durability is determined not only by the qualifications of the implantologist, even if he owns the latest and most advanced techniques, but also by observing the rules of hygiene and care for the finished structures by the patient himself (see below for more on this).
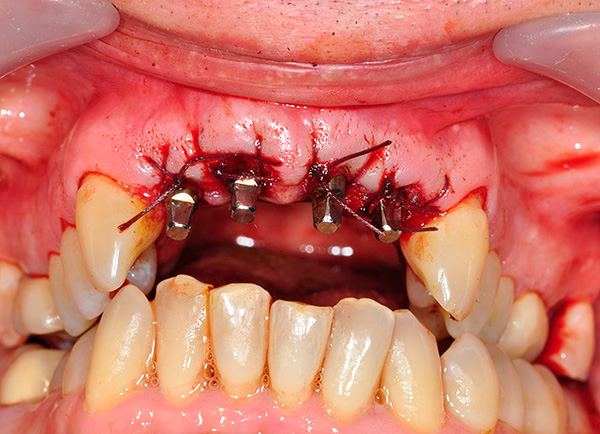
How is the implantation of periodontitis and periodontal disease
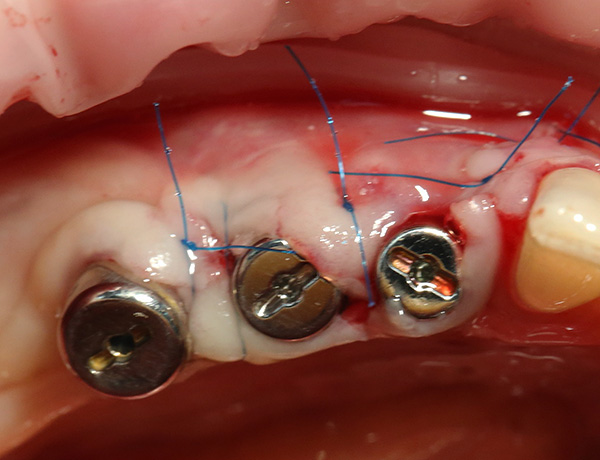
Implantation for periodontitis usually goes through the following stages:
- Preliminary preparation for implantation;
- The choice of implant system;
- Implant Implants;
- Prosthetics on implants.
The preliminary stage is one of the most important, as it allows minimizing the risks during and after implantation. It includes a whole program for the treatment of the underlying disease, that is, periodontitis or periodontal disease. Depending on the possibility of preserving the teeth in the oral cavity, an individualized treatment plan is drawn up.

For example, if we are talking about the preservation of groups of teeth with periodontitis in the initial stage, then preliminary preparation before installing implants can be carried out according to the following scheme:
- Professional teeth cleaning from tartar and plaque;
- Therapeutic (bandages, ointments, etc.), surgical (patchwork operations, curettage, etc.), orthopedic (selective grinding of teeth, splinting, etc.) and orthodontic treatment of periodontitis;
- Removing teeth that are not to be preserved.
Properly performed treatment of the underlying disease can significantly reduce the risk complications after implantation (eg, rejection of dental implants).In the area of installed implants should not be areas of active inflammatory process.
Equally important is the general condition of the oral cavity (level of hygiene, care for the oral cavity) and the formation of correct habits.
But periodontal disease is not always amenable to conservative treatment, and the process of bone atrophy can occur more and more every year. That is why the success of further treatment depends on the tactics of the doctor in each particular case. Most often, preparation for periodontal disease is reduced to the removal of all teeth that are unsuitable for functional and aesthetic indications, followed by implantation and prosthetics.
Of particular interest is the choice of methods for implantation in the presence of periodontitis or periodontal disease. At the moment, implantologists usually choose the following options:
- Classical implantation;
- Express method;
- Basal implantation.
What technologies and implant systems are better suited
Each of the above three implantation technologies is selected for a specific patient, taking into account the severity of periodontitis or periodontal disease. In addition to the degree of atrophy of bone tissue, the doctor also takes into account the patient's age, the presence of associated diseases, features of the maxillofacial area, etc.It is an integrated approach at the initial stage (diagnostics) that allows you to choose the right way to install implants.
Modern clinics in view of the above points most often lean towards the express method and basal implantation. The fact is that the classical implantation is a two-step process and is carried out not immediately after the extraction of the tooth. And after the implants are implanted, more than one month passes before the doctor proceeds with prosthetics.
In contrast to the classical implantation, the express method allows even for periodontitis or periodontal disease (according to indications) to carry out a one-stage implantation immediately after tooth extraction. This speeds up the process of bone regeneration, reduces the level of invasiveness of the intervention and the risk of infection of an open wound. However, for the express method, it is especially important to observe all the technical nuances, which are numerous, and to exercise careful control during the installation of implants.
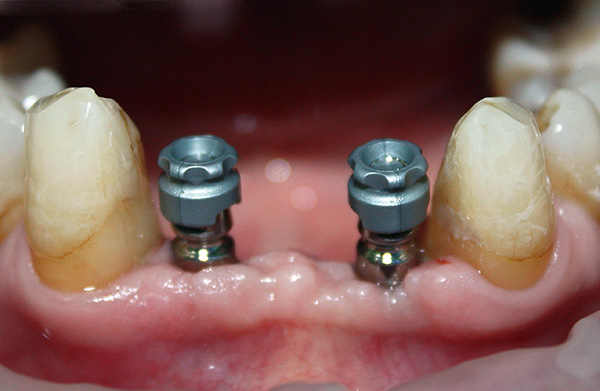
As for the basal implantation, it is used for atrophy of the bone tissue, which often accompanies periodontitis and periodontal disease. Sometimes only this technique is suitable for a significant loss of bone tissue.Such implants are implanted immediately with the abutment (transitional part, on which the prosthesis or crown is fixed) at an angle to where the bone tissue is sufficient for maximum stability.

The structure and shape of the basal implants can withstand heavy loads and stop further bone atrophy. After 5-7 days, it is necessary to make prostheses, which should give an immediate load. Such a short period from implantation to prosthetics gives the basal implants significant advantages - many patients are very happy to get a beautiful smile just a few days after the extraction of teeth.
On a note
Classical types of implantation can be performed even with significant bone atrophy, but with a preliminary sinus lift operation: if there is not enough bone to fix the implant or it is too “loose”, then the dentist first builds up bone tissue (sinus lift) in areas where implants will be installed in the future. As soon as the recovery period is over, the doctor establishes them and then works according to the standard treatment protocol, up to the final prosthetic after 4-9 months (sometimes 1-1.5 years), depending on the specific clinical case.
The choice of an implant system is a crucial stage to which you should approach in a serious way. Today, when choosing a particular type of implant, three main criteria are guided by: guarantee, stability, cost.

To date, there is a kind of implant rating according to these criteria.
For example, premium implants include the following implants:
- Astra Tech (Astra Tech) - implant system from Sweden. Today it is one of the most sought-after due to its excellent technical characteristics, ease of use and, most importantly, a long-term guarantee and stability of engraftment;
- Nobel Biocare - one of the most expensive designs, which is of high quality. This type of implant is suitable for different clinical situations;
- XIVE (Ksaive, Germany). Also very high quality implants;
- Anthogyr is the French system.
And some others.
Medium price level implants - for example:
- Schutz (Germany) - collapsible and non-collapsible structures;
- Zimmer (USA) - mini implants, standard varieties, as well as implants for implantation in a thin bone;
- Niko - Russian implant systems, which are created from German components.
Some implant systems from Israel (for example, AlphaBio) are widely heard among many practicing doctors and are in demand among the Russian population because of the relatively low price. In quality in certain clinical situations, they are not inferior to the most expensive implants from Germany and Sweden.
With regard to Chinese, some Russian and Ukrainian implant systems, many dentists are skeptical about the dubious characteristics and average stability, although there are more than one hundred implantologists who successfully install thousands of similar structures every year. As they say, how many people - so many opinions.
Features of implant care at home: how to prevent periodontitis from continuing its destructive work
The success of prosthetics on implants is influenced not only by the preparation and installation stages of implants, but also by postoperative home care of the structures. This is especially important with persistent periodontitis or periodontal disease, when the success of implantation is directly dependent on the implementation of special rules.

Rule number 1.
Dental implants need more thorough hygiene, since the risk of developing periodontitis in their area is significantly higher than in the case of native teeth. It is especially important to treat the back of the implant, where plaque is formed to a greater degree. Poor hygiene creates an additional risk of rejection.
Rule number 2.
Contact (interdental) surfaces should be cleaned with dental floss. However, some dentists treat such threads negatively as risk factors for permanent injury to the gums due to inept use, so they are inclined to other methods of cleansing the gaps, for example, using interdental brushes or irrigators. Moreover, the irrigator allows not only to successfully clean even the most remote and hard-to-reach areas, where a lot of food debris accumulates, but also improves blood supply in the gums, massaging them.
Rule number 3.
It is important to visit the dentist at least once every 6 months for professional cleaning of teeth and dental implants along with the structures.
It is especially important to follow the recommendations of the doctor in the first postoperative stages, when any small thing is important.For example, in almost all clinical cases, the first time after installing implants (especially with periodontitis and periodontal disease) you cannot smoke, take alcohol, play sports and do hard physical labor. It is necessary to adhere to a sparing diet, take the necessary medications and carry out, in addition to cleaning the teeth from plaque, antiseptic mouth rinses.
All this allows to significantly increase the service life of implants, including life-long operation without any problems.
Be healthy!
An interesting video: what to choose, implantation or classical prosthetics?
About the stages and complications of periodontal disease, as well as about implantation in this disease





Very informative article, all competently, all the pros and cons. Loved it.
Five years ago, gums began to bleed. I went to the dentist, he advised me to buy a conditioner. At the same time, she has already sealed the already exposed tooth root. Every year I went with one problem to the dentist - the fillings fell out and the gums were bleeding. Until they came full tryndets. And now they offer implantation, the issue price is 300-400 thousand. And all the villains in white coats are not treated in urban dentistry, but they offer to go to the paid, where they also earn money (burn them in hell with a blue flame).
Well done
I liked the article, everything is detailed. I was just concerned about the issue of implantation in periodontitis - the doctor offers a bridge, but after reading this article, I learnedthat the abutment teeth of the bridge can also fall out during periodontitis. Thank you very much for the good article!