
Chronic pulpitis may be the outcome of the acute stage of inflammation of the soft tissues inside the tooth, or an independent disease, but regardless of the cause, is perhaps the most insidious form of pulpitis. If at the onset of acute pain, many people quickly turn for help, then with chronic pulpitis the symptoms most often are not pronounced, and sometimes the tooth does not hurt at all.
In this lies the cunning of the disease, since the asymptomatic or lethargic course of the disease sooner or later results in an exacerbation of chronic pulpitis with a palette of unbearable pain, and in the worst - in periodontitis, when it comes to saving a tooth from removal. Moreover, any attempts to endure periodontitis (as often done especially “patient”) often lead to suppuration on the roots - cysts, or to complications of periodontitis - periostitis (“fluxes”), osteomyelitis, abscesses, phlegmon or sepsis, when it comes to about saving a person’s life.

How chronic pulpitis develops, what are its characteristic symptoms, features of recognition, treatment, and prevention of complications - let's talk about that later on.
What is chronic pulpitis?
Generally speaking, pulpitis is an inflammation of the neurovascular bundle within the coronal part of the tooth and root canals. If in acute (focal) pulpitis, in certain cases it is possible to stop the inflammatory process and cure the tooth conservatively, that is, without remove the "nerve"then chronic pulpitis is almost always an irreversible form of the disease. In this case, a gradual degeneration of the pulp occurs inside the tooth: the formation of fibrous tissue, necrosis (necrosis), or the growth of the neurovascular bundle until it fills the carious cavity that led to the pathology.

According to research data in a number of regions, about 75% of visits account for chronic pulpitis, that is, many seek help not because of severe pain symptoms that often do not occur in this form, but because of the fear of losing a tooth. Chronic pulpitis is usually the result of an acute form, although children often develop without it. For the interesting features of acute purulent pulpitis, see a separate article: Characteristic symptoms of acute purulent pulpitis and methods of its treatment.
Chronic forms of pulpitis are caused by pathogenic microorganisms, as well as by their metabolic products, and in most cases the disease is triggered by deep caries or by improper treatment.: violation of the tooth treatment technique, poor cleaning of the carious cavity, poorly applied filling, etc. Less frequent "trigger mechanisms" for the development of pathology are:
- tooth injuries
- channel blockage with calculi (salt plugs)
- penetration of bacteria through the apex of the tooth root in maxillofacial and general diseases (periodontitis, periostitis, osteomyelitis, sinusitis, flu, etc.)

From the practice of the dentist
Surprisingly, some daredevils seriously try to treat pulpitis at home, and not even folk methods are used for this, but simply barbaric methods for the tooth and the body. For example, they take a thin steel needle, heat it red hot and inject it into a deep carious cavity, thereby trying to burn it with the “nerve” inside the tooth. At best, by such an antipotopic method, the acute stage of inflammation will turn into chronic pulpitis.Quite interesting situations are also when trying"Treatment" pulpitis garlic.
By the way, more than 200 years ago, people invented a method of extracting soft tissue from the canals of a tooth using ordinary piano strings. The same string then cleared the channel itself.
Symptoms of chronic pulpitis
As already mentioned, chronic pulpitis, in contrast to acute forms, may be asymptomatic. Acute pulpitis always manifest themselves to be very strong paroxysmal pains with small "light" (not having pain) intervals. For all chronic pulpitis, usually characteristic only aching pain with different intervals of periods without pain.
Most commonly found in dentistry chronic fibrous pulpitis (in almost 70% of cases of appeals), less often - gangrenous. Hypertrophic pulpitis, which is sometimes diagnosed at an appointment with a pediatric dentist, almost never occurs in adults.


Symptoms of chronic fibrous pulpitis (sometimes called chronic simple) are pains from all types of irritants: cold, hot, sweet, from cold air, etc., which persist for a long time after the irritant has been removed.Also for this form of pathology is characterized by such a specific symptom as the occurrence of prolonged pain during the transition from cold to a warm room.
On a note
Chronic simple pulpitis, as diagnosed, is not used by many dentists, as it does not reflect the essence of the degeneration of the structure of the neurovascular bundle in its name. For many practitioners, it is still a question why the classification author Gofung calls fibrous pulpitis chronic simple, because in fact it does not reflect the real picture.
Sometimes chronic fibrous pulpitis is asymptomatic. This is due either to a particular localization of the carious cavity (for example, under the gum), when stimuli cannot affect it, or with a through communication of the cavity and the pulp chamber — in such cases, there is no swelling and swelling of the pulp, and no pain, respectively.
As for chronic gangrenous pulpitisperhaps the most common symptom of this form of the disease is an unpleasant odor that spreads from the tooth. A frequent symptom is also increasing pain from the hot, which does not stop for a long time, even after the irritant is no longer in the mouth. Sometimes there is arching pain in the tooth.
Even if an asymptomatic course is observed, many people note a change in tooth color: the appearance of a grayish tint. As a rule, the appearance of all the listed symptoms of chronic gangrenous pulpitis is preceded by acute and spontaneous pain, which then disappears. This suggests that for many people, the chronic course of the disease is preceded by its acute form.
In chronic hypertrophic pulpitis, the tooth, as a rule, is of minor concern. The main symptom in this case is aching pain when chewing on solid food and rarely from temperature irritants. Sometimes there is a bleeding of the tooth during the meal, which is associated with the growth of pulp in the carious cavity of the “wild meat” type and its mechanical trauma. It is this symptom of chronic pulpitis that often scares a person, forcing him to eventually seek help.
Symptoms of rare pulpitis
In the practice of the dentist, sometimes there are also pulpitis without caries:
- Traumatic;
- Concise;
- Retrograde.
Among them, the most common is traumatic pulpitis - an acute inflammatory process that develops against the background of a tooth injury. Acute tooth trauma occurs when falling (from a bicycle, from a swing), as a result of striking various objects (a washer, balls), etc. In most cases, the upper front teeth are affected, as a result of which there are severe pains from cold and hot, as well as pain when taking solid food.

If the pulp is damaged in case of a tooth injury, then an infection develops acute pulpic pain: long-term and spontaneous, that is, arising even without irritants. As a rule, this happens already within a day. If during this period you do not go to a doctor, then after a while the acute form of traumatic pulpitis may turn into a chronic stage.
Chronic traumatic pulpitis proceeds sluggishly, almost without symptoms. The message of the opened "nerve" with the environment makes it look like a chronic fibrous pulpitis with characteristic signs for it. Without treatment, the chronic form can turn into aggravation or periodontitis (inflammation of the tissues around the tooth root).
Chronic calculitis pulpitis is characterized by slowly increasing symptoms, such as:
- prolonged attacks of pain, sometimes provoked by thermal stimuli (cold, hot);
- long spontaneous pain, sometimes radiating to the ear, temple, cheekbone, neck;
- sometimes pain develops when the head is tilted in one direction or another.
This nature of pain is determined by the reasons for causing it: squeezing of the tooth pulp with denticles or petrifications - stone-like formations. Concretions can be detected in the canals of the tooth using X-ray.
Retrograde pulpitis: has an acute and chronic stage, but differs from classical pulpitis in that it develops without caries. The infection enters the pulp through the apex of the root in diseases such as osteomyelitis, sepsis, sinusitis, and others. In the chronic form, retrograde pulpitis is asymptomatic or with flaccid symptoms.

Timely diagnosis and its significance
In order to diagnose chronic pulpitis, in addition to knowing the history of the disease (complaints, time of occurrence, duration, etc.), the doctor also needs to carry out a complex of diagnostic measures.
The most common additional research methods are:
- visual inspection;
- thermometry;
- EDI;
- radiography.
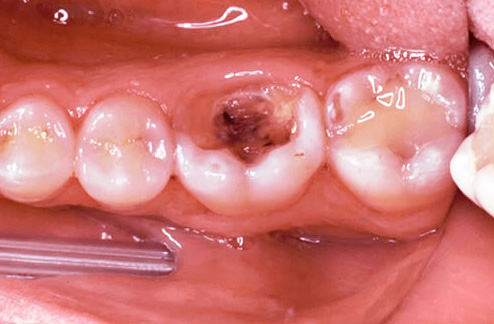
Visual inspection of the tooth with a sharp probe and mirror gives about 50% of the necessary information. By the appearance of the cavity, the painfulness of its bottom, the communication with the pulp chamber (the place where the “nerve” is located) we can already assume chronic pulpitis.

If there is a message with a carious cavity and there is pain and bleeding when probing with a sharp probe, then with high probability this is a chronic fibrous pulpitis. When a tooth changes color, a gray tint appears, with a large amount of softened carious tissue in the cavity of the tooth, when the “nerve” is partially destroyed and pain occurs only when probing channels, then it is most likely chronic gangrenous pulpitis. The appearance of an overgrown tissue inside the carious cavity, combined with soreness when probing it, most often indicates chronic hypertrophic pulpitis.
Thermometry. As an additional study, thermometry is often resorted to - analyzing the reaction of a tooth to a cold one and less often hot.When a tooth reacts to a cold one, it can be safely asserted that the “nerve” inside it did not die, therefore, periodontitis is not in question. For accurate thermometry, you can use special sensors developed by Chepulis and Sirvidene, which capture the temperature difference between a healthy and a sick tooth.
EDI or, alternatively, electrical donation diagnostics is one of the most accurate methods for diagnosing pulpitis. Its principle is based on the various electrical excitability of a healthy and diseased pulp.
A healthy "nerve" is already reacting with weak pains to a current strength of 2-6 μA. Acute forms of pulpitis respond to currents ranging from 20-25 to 35 μA. Chronic fibrous pulpitis is recorded at a current of 35-50 μA, with chronic gangrenous - at 60-90 μA. Chronic hypertrophic pulpitis is not diagnosed by EDI, and radiography is used to refine it.
X-ray is a method based on the study of film X-rays of a tooth with its surrounding tissues transferred to a computer with the help of a device - a visiograph (unless, of course, we are talking about a modern clinic).

To confirm the diagnosis of chronic hypertrophic pulpitis, on the radiograph there should be no changes in the tissues surrounding the tooth and in the region of the interroot septum.The picture of a tooth with chronic fibrous pulp most often also has no changes, but sometimes there is a slight expansion of the periodontal gap (between the root of the tooth and the hole), which complicates the diagnosis. Chronic gangrenous pulpitis is rarely characterized by bone defects in the apex of the roots of the teeth, therefore, the diagnosis is confirmed by thermometry and EDI.
Modern treatment of chronic forms and exacerbations of pulpitis
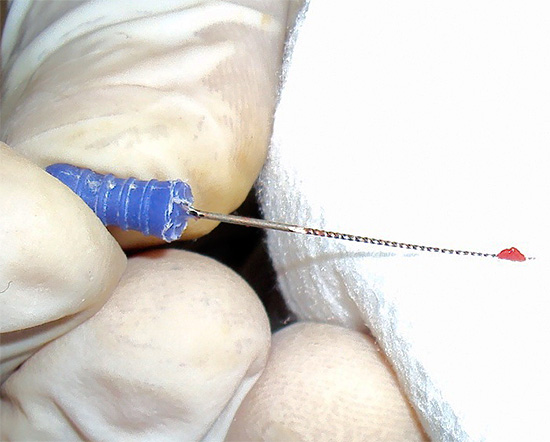
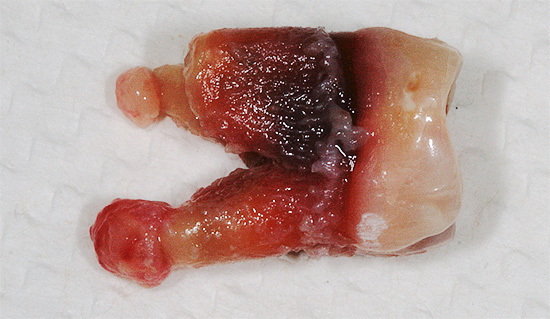
Since chronic pulpitis is an irreversible form of inflammation of soft tissues, when they can no longer be stored in the tooth, they are most often used for treatment. complete extraction of pulp from all dental canals. The same approach is followed in the treatment of chronic pulpitis in the acute stage.

In modern dentistry, preference is given to the method of vital (living) extirpation (extraction) of the “nerve”. During the treatment of chronic forms of pulpitis or its exacerbations, only anesthesia is used without additional means for devitalization (killing) of the pulp.
In a number of institutions, especially budget ones, arsenic paste (“arsenic”) or arsenic-free products is still used to preliminarily prepare the pulp for its extraction in triplicate visits. Anesthesia is also often used, but the lack of time, the inability to bring the anesthesia to perfection, the rush or individual characteristics of the jaw of a particular patient lead to the inability to remove the “nerve” immediately.
Arsenic paste is placed on single-root teeth for 24 hours, on multi-root teeth - for 48 hours. Paste that does not contain arsenic, is placed for a long time: from 2-3 days to a week or more. Unlike arsenic paste, it does not have a detrimental effect on the surrounding root tissue, it acts slowly and gently. That is why it is increasingly often given preference to means that do not contain arsenic.
From the experience of the dentist
Tooth canal treatment is a very important undertaking. Just extracting the “nerves” from the channels is not enough, as many people think. Only prolonged leaching of the entire infection from the canal system, treatment of the inner walls of the roots from infected tissues, and then reliable filling can give good results for the long term.If at least one of these stages is broken, then in the near future pains can occur in the “dead” tooth, and changes will begin to occur in the tissues surrounding the root, up to the beginning of the formation of a “cyst” - a bag filled with pus and bounded by a capsule from healthy bone areas. See also article Tooth cyst removal procedure and its treatment without surgery.
Complications after treatment of chronic pulpitis
After treatment of chronic pulpitis or exacerbation, patients often feel pains that dentists call post-sealing.
On a note
A number of authors are of the opinion that normally such pains should not occur at all, but the imperfection of the technical and professional component allows for minor aching pain immediately after filling (lasts no more than an hour), or pain when biting on a tooth that lasts from 1 to 3 days.
Post-compaction pains that fit into the conditional norm occur due to a slight injury to the tissues surrounding the tooth, with a rough separation of the “nerve” during its extraction, due to the drug treatment of the canal with strong antiseptics,which in small quantities fall outside the root, as well as due to the release of a thin intra-channel instrument beyond the apical opening of the root.

The gross violations of the doctor are:
- poor quality of the canal or channels;
- break off the tool in the channel;
- creating perforations in the channel (hole or damage to the root wall).

If in the treatment of chronic pulpitis or its exacerbations, the channels are not filled up or their excessive filling (removal of material beyond the apex), then immediately or after some time (from a day to a year or more) symptoms occur that correspond to periodontitis in an exacerbation. This can most often be acute pain, the inability to touch the tooth even with the tongue, the pulsating nature of the pain, and in some cases, after some time, swelling of the mucous membrane in the area of the apex of the tooth root may occur.
When the instrument breaks off in the canal, the tooth may not manifest itself for a long time, but sooner or later the infection in the “not sore” and not filled root area will cause either a purulent process in the canal with the formation of a “flux” or the process will have a chronic form with the formation of fistula (ducts,opening on the gum, through which pus from the root of the tooth is secreted into the oral cavity), and at worst - the formation of purulent sacs - cysts.
Perforation, or, in a different way, “hole” in the root, almost always manifests itself immediately. Often the patient himself notices when the doctor mistakenly went instead of the canal into the “gum”. As a rule, in a few hours after such treatment of chronic pulpitis or exacerbations, severe aching pain or acute paroxysmal pain occurs. Sometimes even painkillers may not help.
Let's summarize a little ...
At the first symptoms of chronic pulpitis or its exacerbation, you should immediately consult a doctor. 100% guarantee that during treatment there will be no complication, no clinic can, but many of them have a special approach to the treatment of chronic and other pulpitis, which make these risks minimal.
For example, many expensive dental clinics pay great attention to intracanal treatment of chronic pulpitis, devoting at least 1 hour to this procedure (to a single canal tooth). Budget organizations can not boast such a margin of time for only one mechanical and drug treatment channels and their filling.But any rush increases the risk of complications ...
The leading importance in the prevention of complications is played by the professional training of a dentist and the level of equipment of the clinic. Therefore, it is important before treatment to get as much information as possible from relatives and friends about the clinic and its doctors. The right choice of institution and doctor will allow to successfully treat and fill the canals, keeping the tooth for many years.
An interesting video about the causes of pulpitis and its potential danger.
An exciting example of removing a broken instrument from a dental canal.



